Revolutionizing Pulmonary Embolism Treatment: A New Era
As a blogger who is passionate about health and science, I am always excited to share the latest breakthroughs in medical research. In this article, I will discuss the future of pulmonary embolism treatment, focusing on the advances in research and medicine that are revolutionizing the way we approach this life-threatening condition. So, let's dive into the fascinating world of medical innovation and explore the various ways that these cutting-edge advancements are shaping the future of pulmonary embolism treatment.
The Role of Artificial Intelligence in Diagnosing Pulmonary Embolism
Artificial intelligence (AI) has been making waves in the medical field, and its impact on the diagnosis of pulmonary embolism is no exception. With the help of AI, doctors are now able to analyze complex medical images and data more accurately and swiftly than ever before. This not only enables early detection of pulmonary embolism, but also allows for more personalized treatment plans tailored to the individual patient's needs. As AI continues to advance, we can expect even more precise and efficient diagnostic tools that will significantly improve the management of pulmonary embolism.
Novel Anticoagulant Therapies: A Game Changer in Treatment
Anticoagulant medications, also known as blood thinners, have long been the cornerstone of pulmonary embolism treatment. However, recent advancements in pharmacology have led to the development of novel anticoagulants that boast fewer side effects and more convenient dosing schedules. These new drugs, such as direct oral anticoagulants (DOACs), have the potential to revolutionize the way we treat pulmonary embolism by offering patients a safer and more manageable alternative to traditional anticoagulant therapy.
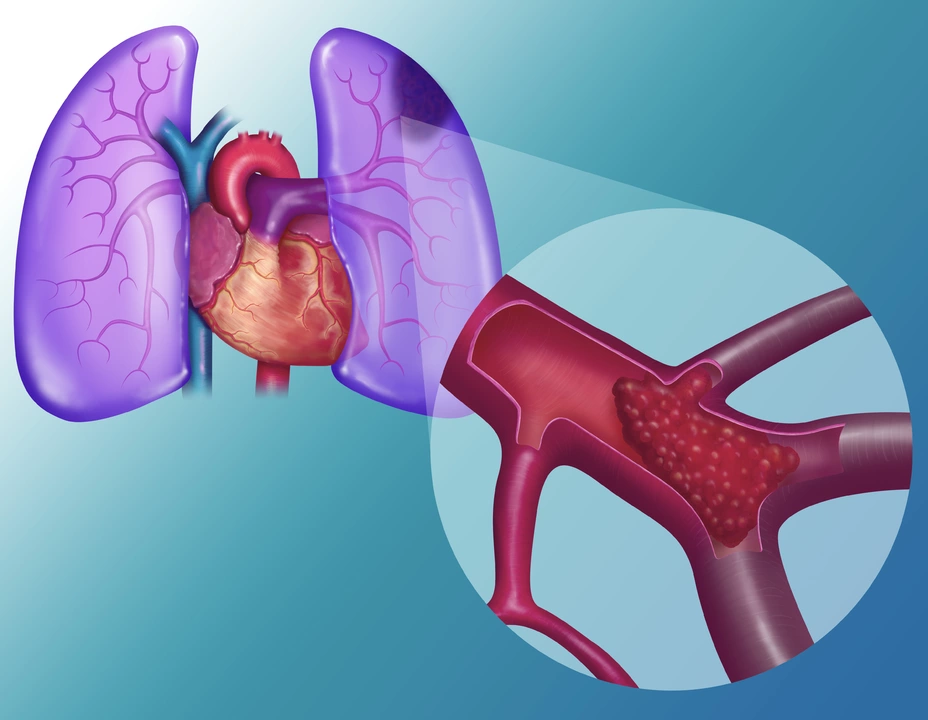
Advancements in Interventional Radiology: Minimally Invasive Solutions
Interventional radiology is a rapidly evolving field that offers minimally invasive solutions for various medical conditions, including pulmonary embolism. Through the use of advanced imaging techniques, doctors can now perform intricate procedures such as catheter-directed thrombolysis, which involves the targeted delivery of clot-dissolving drugs directly to the site of the embolism. This minimally invasive approach not only reduces the risk of complications, but also shortens the recovery period, making it an increasingly popular option for treating pulmonary embolism.
Breaking New Ground with Pulmonary Embolism Response Teams (PERT)
As the medical community continues to recognize the importance of a multidisciplinary approach to healthcare, the concept of pulmonary embolism response teams (PERT) has emerged as a promising strategy for improving patient outcomes. PERT brings together specialists from various fields, such as cardiology, pulmonology, and interventional radiology, to work collaboratively in the diagnosis, management, and treatment of pulmonary embolism. By fostering better communication and coordination among healthcare providers, PERT has the potential to significantly enhance the quality of care for patients with pulmonary embolism.
Exploring the Potential of Biomarkers for Risk Stratification
Biomarkers are measurable substances in the body that can help doctors assess a patient's risk of developing certain medical conditions, including pulmonary embolism. Recent research has shed light on the potential of various biomarkers, such as D-dimer and high-sensitivity cardiac troponin, to aid in the risk stratification and management of pulmonary embolism. As our understanding of these biomarkers continues to grow, they may play an increasingly important role in guiding clinical decision-making and ensuring that patients receive the most appropriate and effective treatment.
Personalized Medicine: Tailoring Treatment to the Individual Patient
One of the most exciting advancements in the field of pulmonary embolism treatment is the move towards personalized medicine. By taking into account factors such as genetics, lifestyle, and comorbidities, doctors can now develop individualized treatment plans that are tailored to the specific needs of each patient. This customized approach not only enhances the effectiveness of treatment, but also minimizes the risk of side effects and complications, ultimately leading to better patient outcomes.
Advancing Our Understanding of the Genetic Basis of Pulmonary Embolism
The field of genetics has made significant strides in recent years, and these advances are beginning to shed light on the genetic basis of pulmonary embolism. By identifying the specific genes and genetic mutations that contribute to the development of this condition, researchers are opening the door to the development of targeted therapies and preventative measures that could revolutionize the way we approach pulmonary embolism treatment.
Prevention Strategies: The Key to Reducing the Burden of Pulmonary Embolism
As the old saying goes, prevention is the best medicine. In the case of pulmonary embolism, recent research has highlighted the importance of various prevention strategies, such as exercise, weight management, and smoking cessation, in reducing the risk of this life-threatening condition. By educating patients and promoting healthy lifestyle choices, healthcare providers can play a crucial role in preventing the occurrence of pulmonary embolism and ultimately reducing the overall burden of this devastating disease.
Looking to the Future: What's on the Horizon for Pulmonary Embolism Treatment?
As we look towards the future, it is clear that the field of pulmonary embolism treatment is on the cusp of a new era. With advancements in AI, novel anticoagulant therapies, interventional radiology, and personalized medicine, we are witnessing a transformation in the way we diagnose, manage, and treat this life-threatening condition. As researchers continue to break new ground and push the boundaries of what is possible, there is no doubt that we will see even more innovative and groundbreaking advancements in the years to come.

11 Comments
Christopher Montenegro
13 May, 2023Your optimistic portrayal utterly disregards the entrenched uncertainties plaguing pulmonary embolism therapeutics.
Kyle Olsen
23 May, 2023While you have illuminated the superficial allure of artificial intelligence in pulmonary embolism diagnostics, the underlying methodological frailties remain starkly evident. The purported precision of algorithmic interpretation is often confounded by heterogeneous imaging protocols, rendering cross‑institutional validation a Sisyphean endeavor. Moreover, the seductive narrative surrounding novel anticoagulants neglects the rigorous pharmacovigilance datasets that continue to expose latent hemorrhagic risks. One must also acknowledge that interventional radiology, despite its minimally invasive veneer, is not immune to operator‑dependent variability. In sum, the current discourse exaggerates incremental gains while masking profound epistemic gaps.
Sarah Kherbouche
1 June, 2023Honestly, this whole hype train about PERT teams feels like another American‑centric gimmick that ignores the gritty reality of our overburdened hospitals. The so‑called “multidisciplinary” approach often devolves into bureaucratic red‑tape, delaying life‑saving interventions for patients who can’t wait for endless committee meetings. And don’t get me started on the “personalized medicine” buzzword – it’s just a fancy label for expensive drugs that most folks can’t afford.
MANAS MISHRA
10 June, 2023I see your point about methodological challenges, and it’s true that AI models need robust, standardized imaging data to truly shine. Yet, there have been promising multi‑center studies that demonstrate improved sensitivity when algorithms are trained on diverse cohorts. Additionally, while operator skill does influence outcomes in catheter‑direct therapies, standardized training protocols are gradually narrowing that gap. Balancing enthusiasm with cautious appraisal will help us harness these innovations responsibly.
Lawrence Bergfeld
19 June, 2023Great observation!; however, consider that many institutions are already piloting streamlined PERT workflows, which have shown reduced door‑to‑treatment times.; with proper resource allocation, the bureaucratic hurdles you mention can be mitigated.; The key is focused implementation.
Chelsea Kerr
29 June, 2023🌟 The trajectory of pulmonary embolism treatment reads like a microcosm of modern medicine’s quest for precision and humanity intertwined. 🧬 As we decode genetic predispositions, we uncover layers of biological nuance that were previously cloaked in mystery. 🤔 The integration of AI-driven imaging not only accelerates diagnosis but also invites us to reconsider the clinician’s role as a data interpreter rather than a sole arbiter of truth. 📊 Novel oral anticoagulants, while promising, still demand rigorous post‑marketing surveillance to ensure safety across diverse populations. 🚑 Interventional radiology’s evolution toward catheter‑directed therapies exemplifies how minimally invasive techniques can reduce morbidity without sacrificing efficacy. 🌐 Multidisciplinary Pulmonary Embolism Response Teams (PERT) embody a collaborative ethos, yet their success hinges on seamless communication and shared decision‑making. 🗣️ Biomarkers such as high‑sensitivity troponin and D‑dimer are becoming indispensable tools for risk stratification, guiding clinicians toward tailored interventions. 🧪 Personalized medicine, grounded in genomic insights and lifestyle factors, promises to align therapeutic intensity with individual risk profiles. 💡 Yet, the ethical dimensions of genetic screening-privacy, consent, and equitable access-remain unresolved. 🌱 Preventative strategies, from promoting physical activity to smoking cessation, underscore the timeless adage that prevention outweighs cure. 🌍 Public health initiatives must therefore be woven into the fabric of clinical practice to mitigate the global burden of embolic disease. 🏥 Education of patients and providers alike fuels empowerment, transforming passive recipients into active participants in care. 📚 As research pushes the boundaries of what is possible, humility must temper our optimism, acknowledging that each breakthrough introduces new complexities. 🤝 Ultimately, the future of pulmonary embolism treatment will be defined not solely by technological marvels, but by our collective capacity to integrate science with compassion. 🌈
Tom Becker
8 July, 2023Yo, before we get blinded by shiny AI toys and fancy gene panels, remember who's really pulling the strings-big pharma and tech giants. They’ll push "personalized" meds so we all get hooked on pricey subscriptions while the real cure stays hidden in the shadows. And those PERT teams? Just another way to funnel billions into bureaucratic layers that profit the elite, not the patient. Don’t be fooled by the glossy press releases; the data is often cherry‑picked, and the side‑effects are buried deep in fine print you’ll never see.
Laura Sanders
17 July, 2023Honestly the hype around biomarkers is overblown. D‑dimer is old news and troponin isn’t specific enough to revolutionise care. We need real innovation not just re‑packaging of existing tests.
Jai Patel
26 July, 2023Hey Laura, I get where you’re coming from, but think of it this way-biomarkers are like the secret spices in a grand culinary masterpiece! 🌶️ When combined with AI analytics, they can reveal patterns that were invisible before, turning a bland diagnosis into a vibrant, data‑rich narrative. Plus, they empower clinicians in resource‑limited settings to make smarter, faster decisions.
Zara @WSLab
5 August, 2023Great rundown! 🌟 I’m especially curious about how interventional radiology procedures are being standardized across different hospital systems. Consistency in training could really make a difference in patient outcomes.
Randy Pierson
14 August, 2023Indeed, Zara! Uniform protocols and simulation‑based curricula are vital for reducing operator‑dependent variability. By establishing clear competency benchmarks, we can ensure that every patient benefits from the latest minimally invasive techniques, regardless of geography.