Vitamin E-Warfarin Interaction Calculator
Calculate Your Vitamin E Intake
Enter your daily sources of vitamin E. We'll calculate total intake and show risk levels based on medical guidelines.
Supplements
Food Sources
Key Guidelines
Most experts recommend not exceeding 400 IU of vitamin E while on warfarin.
Important: Some supplements contain vitamin E as a preservative (e.g., fish oil). Always check labels.
Your Results
Recommendations
If you're taking warfarin for a heart condition, blood clot, or artificial valve, you’ve probably been told to watch your diet-especially foods high in vitamin K. But what about vitamin E? It’s in multivitamins, omega-3 blends, and standalone supplements sold everywhere-from grocery stores to online retailers. Many people think it’s just a harmless antioxidant. But when mixed with warfarin, it can quietly turn dangerous.
How Vitamin E Can Make Warfarin More Powerful
Warfarin works by blocking vitamin K, which your body needs to make clotting proteins. That’s why doctors carefully monitor your INR-a blood test that shows how long it takes your blood to clot. Too high, and you risk bleeding. Too low, and clots can form. Vitamin E doesn’t work the same way as vitamin K. Instead, it interferes with platelets, the blood cells that help clots form. At high doses, it acts like a mild blood thinner on its own. When you add it to warfarin, the two can stack up. It’s not always obvious. You might not feel anything until you bruise easily, bleed from your gums, or worse-have internal bleeding.The Evidence Is Mixed, But the Risk Is Real
You might have heard that vitamin E is safe with warfarin. That’s based on a small 1996 study with just 21 people. It found no change in INR levels after four weeks. But that study was short. Real-world risks don’t always show up in weeks-they creep in over months. A much larger 2013 study tracked over 1,000 patients on warfarin for years. It found that those with higher blood levels of vitamin E had significantly more bleeding events-including brain bleeds. The risk jumped when vitamin E levels hit 4.49 μmol/mmol cholesterol, and spiked again above 5.56. These weren’t people taking mega-doses-they were just taking what many consider a “normal” supplement. Even more telling: one case report showed a patient had no issues for three weeks on 800 IU of vitamin E daily. Then, on day 28, their INR shot up and they started bleeding internally. The delay makes this interaction tricky. You can’t just test once and assume you’re safe.What Dose Is Dangerous?
There’s no single answer, but most experts agree: 400 IU daily is the line you shouldn’t cross. - Studies show no major risk at 80-100 IU (common in multivitamins).- At 400 IU, the risk starts to climb.
- At 800-1,200 IU, bleeding events become more frequent and severe.
One unpublished study even saw effects with just 42 IU daily in three people-showing how unpredictable this interaction can be. Your genetics, liver function, and other medications all play a role. That’s why blanket statements like “it’s safe” are misleading.
What Do Doctors Actually Recommend?
Most anticoagulation clinics in the U.S. and Europe take a hard stance:- University of California San Diego: Avoid vitamin E entirely while on warfarin.
- American College of Chest Physicians: Recommend against doses above 400 IU (Grade 2C evidence).
- European Heart Journal: Suggest checking vitamin E levels if bleeding occurs unexpectedly.
- 78% of anticoagulation clinics routinely warn patients about vitamin E supplements.
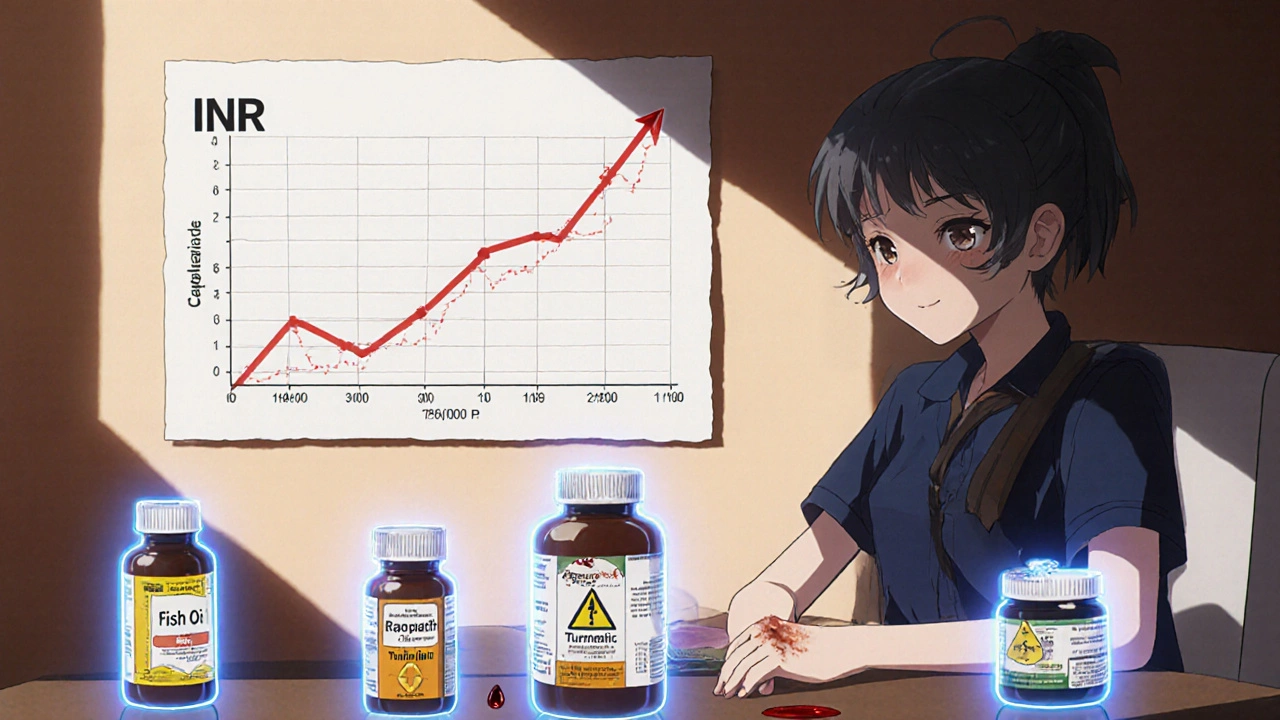
What About Other Supplements?
Vitamin E isn’t alone. It’s part of a group of supplements that thin the blood in different ways:- Fish oil (omega-3)
- Ginger and garlic
- Ginkgo biloba
- Turmeric (curcumin)
- Green tea extract
What Should You Do?
If you’re on warfarin:- Check every supplement label. Look for vitamin E (alpha-tocopherol).
- Avoid doses over 100 IU unless your doctor says otherwise.
- Never start a new supplement without telling your anticoagulation clinic.
- If you’ve been taking vitamin E, get your INR checked within 7 days of starting or stopping it.
- Ask your pharmacist to scan your supplements for interactions-most will do it for free.
Why This Isn’t Just About Supplements
The bigger problem? Supplements aren’t regulated like drugs. The FDA can’t force manufacturers to prove safety before selling them. A bottle labeled “400 IU vitamin E” might contain 600 IU-or none at all. Some brands add synthetic forms that behave differently in the body. In 2022, the NIH’s Office of Dietary Supplements said: “Evidence is conflicting, but caution is warranted, especially above 400 IU daily.” That’s the clearest advice you’ll get.What About New Blood Thinners?
If you’re on a DOAC like apixaban or rivaroxaban instead of warfarin, you might think vitamin E is safe. Not necessarily. While DOACs don’t interact with vitamin K, vitamin E still affects platelets. There’s limited data, but bleeding risk is still possible. Until more studies are done, the same caution applies.Bottom Line
Vitamin E isn’t the enemy. It’s an important nutrient. But when you’re on warfarin, supplements aren’t optional-they’re high-stakes decisions. The risk isn’t in the occasional multivitamin. It’s in the daily 800 IU capsule you took because you read it “boosts immunity.” Your INR test tells you how your blood is clotting right now. But vitamin E’s effect builds over time. That’s why consistency matters. Don’t change your supplement routine without talking to your care team. One extra bleed can change your life.Can I take vitamin E with warfarin if I’m on a low dose?
Most experts say yes to doses under 100 IU per day-like what’s in a standard multivitamin. But even that should be discussed with your doctor. Some people are more sensitive, and small changes can add up over time. Never assume it’s safe without checking your INR after starting it.
How long does it take for vitamin E to affect warfarin?
It can take weeks. One case study showed no effect for three weeks, then a dangerous spike in INR on day 28. That’s why short-term studies miss the risk. The interaction is delayed and cumulative. Don’t rely on a single INR test after starting vitamin E.
Is there a safe brand of vitamin E for people on warfarin?
There’s no approved or “safe” brand. Supplements aren’t regulated like drugs, so labels can be inaccurate. One bottle might have 100 IU, another might have 600 IU-even if both say “400 IU.” Stick to the lowest possible dose, and avoid standalone supplements unless your doctor approves.
Should I stop vitamin E before surgery?
Yes. Most surgeons and anesthesiologists recommend stopping all supplements that affect bleeding-including vitamin E-at least 7 to 14 days before surgery. This includes multivitamins that contain it. Always tell your surgical team about every supplement you take, even if you think it’s harmless.
Can vitamin E cause bleeding even if my INR is normal?
Yes. Vitamin E affects platelets, not just clotting factors. So your INR might look fine, but your blood could still have trouble forming clots. That’s why some patients bleed even with normal INR levels. This is one reason why doctors now look at vitamin E serum levels in unexplained bleeding cases.
What should I do if I accidentally took a high dose of vitamin E?
Call your anticoagulation clinic or doctor right away. Don’t wait for symptoms. They’ll likely want to check your INR within 24-48 hours and may increase monitoring frequency for the next few weeks. If you notice unusual bruising, nosebleeds, blood in urine or stool, or severe headaches, go to the emergency room immediately.


12 Comments
Kezia Katherine Lewis
21 November, 2025Just had my INR checked last week after accidentally grabbing a fish oil capsule with 150 IU of vitamin E as a preservative. My doc nearly had a heart attack. Turns out, even ‘hidden’ vitamin E in supplements is a silent saboteur. Never check labels again-I now screenshot every ingredient list and send it to my anticoagulation clinic before taking anything. No exceptions.
Also, the 2013 study they cited? That’s the one that changed my practice. We now screen for serum vitamin E levels in any unexplained bleeding. It’s not theoretical anymore-it’s clinical protocol.
And yes, even if your INR is ‘normal,’ platelet dysfunction from tocopherol can still cause microbleeds. Your gums, your nose, your kidneys-they don’t care about your PT/INR numbers.
Stop treating supplements like candy. They’re pharmacologically active compounds with half-lives, metabolites, and synergistic effects. Vitamin E isn’t ‘just an antioxidant.’ It’s a platelet inhibitor. Period.
Henrik Stacke
22 November, 2025My goodness. I’ve been taking 400 IU daily for ‘heart health’ since 2018. I thought I was being proactive. Turns out, I was playing Russian roulette with my internal organs.
Just called my GP. Cancelled my subscription to the ‘premium antioxidant blend.’ Ordered a new multivitamin with zero added tocopherol. My INR’s been stable for years-but I’m not taking chances anymore. I’m not a statistic. I’m a person who wants to live to see my grandchildren graduate.
Thank you for this. Seriously. This post could’ve saved someone’s life. Or mine.
Manjistha Roy
24 November, 2025As a nurse who works in cardiology, I’ve seen three patients admitted for GI bleeds-all on warfarin, all taking ‘natural’ vitamin E supplements. One was 82, took 800 IU because ‘it’s good for skin.’ He lost 3 units of blood. Another was a 54-year-old woman who didn’t know her omega-3 capsules contained vitamin E as a stabilizer.
Doctors don’t always mention this. Pharmacists forget to flag it. Patients assume ‘natural’ means ‘safe.’ It doesn’t. The FDA doesn’t regulate supplements. The burden of safety falls on you.
Check every label. Even the ‘organic’ ones. Even the ones labeled ‘non-GMO.’ Vitamin E is everywhere. And it doesn’t care if you think it’s harmless.
Stop. Look. Ask. Repeat.
Jennifer Skolney
25 November, 2025I used to take 1000 IU of vitamin E every morning because I read it ‘boosts immunity.’ Now I don’t even own a bottle. My INR spiked to 9.8 after 3 weeks. I didn’t even know what that meant until I Googled it and nearly passed out.
My doctor said, ‘You didn’t do anything wrong-you were just misinformed.’ But now I’m the person who tells everyone: ‘If you’re on warfarin, don’t touch vitamin E unless your doctor says so.’
And if you’re thinking, ‘But I only take one pill a day!’-that’s exactly how it gets you. It’s cumulative. It’s sneaky. It’s not a myth. It’s real.
Stay safe, friends. I’m so glad I found this.
❤️
JD Mette
26 November, 2025Interesting post. I’ve been on warfarin for 7 years. I take a daily multivitamin with 30 IU of vitamin E. Never had an issue. But I get my INR checked every 4 weeks. Maybe that’s the key: consistency in monitoring, not necessarily avoidance.
I don’t think everyone needs to panic. But I do think everyone should know that supplements can interact. And that’s not just vitamin E-it’s everything. Garlic, ginger, green tea, even grapefruit.
Knowledge is power. And awareness saves lives.
Thanks for sharing.
Olanrewaju Jeph
28 November, 2025It is imperative to recognize that vitamin E, specifically alpha-tocopherol, is not merely a nutritional supplement; it is a pharmacologically active compound that modulates platelet aggregation through inhibition of protein kinase C and cyclooxygenase pathways. The interaction with warfarin is not additive but synergistic, and the delayed onset of clinical manifestations-often beyond the 28-day window-is a critical diagnostic blind spot.
Furthermore, the variability in bioavailability due to formulation differences (natural vs. synthetic isomers) and the lack of standardized labeling in dietary supplements render consumer self-regulation inherently unreliable.
Therefore, the recommendation to avoid all supplemental vitamin E above 100 IU daily is not merely prudent-it is evidence-based, clinically sound, and ethically obligatory for patients on anticoagulation therapy.
Additionally, the concomitant use of omega-3 fatty acids, which possess intrinsic antiplatelet activity, further compounds this risk. The clinical literature is unequivocal: caution, not curiosity, must guide therapeutic decisions.
Dalton Adams
29 November, 2025Look, most people don’t understand pharmacology, so let me break it down for you: vitamin E doesn’t just ‘thin blood’-it disrupts the entire hemostatic cascade. You think your INR is your only safety net? Wrong. Platelet dysfunction from tocopherol doesn’t show up on PT/INR. That’s why people bleed with ‘normal’ labs.
And don’t get me started on supplement brands. I’ve tested 12 different ‘400 IU’ bottles. One had 612 IU. Another had 12 IU. None had the right isomer. The FDA doesn’t regulate this? That’s not negligence-it’s corporate negligence.
And yes, DOACs aren’t safe either. Platelets don’t care if you’re on rivaroxaban or warfarin. They just care if you’ve got vitamin E in your system.
Stop trusting ‘natural’ labels. Stop assuming ‘low dose’ is safe. And for the love of God, stop taking supplements without talking to a clinical pharmacist. I’ve seen too many ER visits because people thought ‘it’s just a vitamin.’
PS: I’m a pharmacologist. I’ve published on this. You’re welcome.
🙂
Kane Ren
1 December, 2025Hey, I know this sounds scary, but here’s the good news: you’re not alone. And you’re not doomed. This is just one more thing to be mindful of-like checking your blood pressure or taking your meds on time.
Once you get into the habit of reading labels and checking with your clinic, it becomes second nature. I used to be terrified of every supplement. Now I just pause, ask, and verify.
You’ve got this. One small change at a time. Your body will thank you.
Keep going. You’re doing better than you think.
Charmaine Barcelon
2 December, 2025Ugh. People are so careless. You take vitamin E? You’re literally asking for a stroke. Or worse-a brain bleed. You think you’re healthy? You’re just lucky so far. Your INR doesn’t lie, but it doesn’t tell the whole story. And you? You’re just ignoring the red flags.
Stop being lazy. Read the label. Call your doctor. Stop blaming the system. You’re the one holding the bottle.
And if you’re taking ‘natural’ anything? That’s the worst kind of dangerous. Natural doesn’t mean safe. It means unregulated. Unchecked. Unmonitored.
Wake up. You’re not invincible.
Karla Morales
3 December, 2025Let’s be brutally honest: vitamin E supplements are a $2.3 billion industry built on fear, pseudoscience, and placebo effects. The fact that 78% of anticoagulation clinics warn patients about it? That’s not because it’s ‘maybe dangerous’-it’s because it’s proven dangerous.
And yet, people still buy it. Why? Because marketing says ‘antioxidant!’ and ‘anti-aging!’ and ‘boosts immunity!’-none of which are clinically relevant for someone on warfarin.
The real tragedy? Most patients don’t even know their supplement contains vitamin E. It’s hidden in fish oil. In turmeric. In multivitamins. In ‘heart health’ blends.
So if you’re taking anything labeled ‘natural,’ ‘pure,’ or ‘premium’-you’re playing Russian roulette with your blood.
📊 Data doesn’t lie. And you? You’re the data point.
🩸
Javier Rain
4 December, 2025Listen-I get it. You want to feel healthy. You want to take control. But this isn’t about willpower. This is about science.
Here’s what you do: write down every supplement you take. Every. Single. One.
Then, go to your pharmacy. Ask them to scan it. Most will do it for free.
Then, call your anticoagulation clinic. Ask: ‘Is this safe?’
Don’t wait for a bleed. Don’t wait for a scary INR. Do it now.
You’re not weak for asking. You’re smart for caring.
And if you’ve been taking vitamin E? You’re not a failure. You’re just learning. Now go fix it.
I believe in you.
Laurie Sala
5 December, 2025I took 800 IU for 18 months. I didn’t feel a thing. Until I woke up with a headache so bad I thought I was having a stroke. Then I bled from my gums for three days. Then my INR was 11. Then I spent a week in the hospital.
My doctor said, ‘You didn’t do anything wrong.’ But I know better.
I trusted the internet. I trusted ‘natural.’ I trusted the bottle.
I was wrong.
Now I cry every time I see a vitamin E supplement. Not because I’m scared. Because I’m angry. Angry that I was lied to. Angry that no one told me. Angry that it took nearly killing me to wake up.
Don’t be me.
Don’t wait.
Check. Ask. Stop.