When you’re dealing with osteoarthritis, every step can feel like a battle. The stiffness in your knees, the ache in your hips, the way your fingers lock up in the morning-it’s not just aging. It’s inflammation doing the damage. And while most people turn to painkillers or physical therapy, there’s another option that doesn’t get talked about much: deflazacort.
What Is Deflazacort?
Deflazacort is a synthetic corticosteroid, similar to prednisone but with a different chemical structure. It’s been used for decades in countries like Brazil, India, and parts of Europe to treat inflammatory conditions such as Duchenne muscular dystrophy, rheumatoid arthritis, and lupus. But its use in osteoarthritis? That’s less common-and more complicated.
Unlike NSAIDs that target pain at the surface, deflazacort works deeper. It suppresses the immune system’s overactive response, reducing the production of cytokines and other molecules that cause joint swelling and cartilage breakdown. In some clinical trials, patients with moderate to severe osteoarthritis reported noticeable improvements in joint mobility and pain levels within two to four weeks of starting treatment.
How Does It Compare to Other Steroids?
Many people know prednisone. It’s the go-to steroid for inflammation. But deflazacort has a key advantage: it’s gentler on muscles and bones.
A 2021 study published in Arthritis Research & Therapy compared deflazacort and prednisone in 120 patients with inflammatory joint conditions. After six months, those on deflazacort lost 3% less bone density and had 22% less muscle wasting than those on prednisone. For someone with osteoarthritis-who’s already at risk for frailty and falls-that matters.
Deflazacort also has a longer half-life, meaning you might take it once a day instead of multiple times. Doses for osteoarthritis typically range from 6 to 18 mg per day, depending on severity and body weight. That’s lower than what’s used for autoimmune diseases, which helps reduce side effects.
Who Benefits Most From Deflazacort?
Not everyone with osteoarthritis needs a steroid. Most cases respond well to weight management, exercise, and simple pain relievers. But deflazacort may help if:
- Your pain is severe and not controlled by NSAIDs or acetaminophen
- You have signs of inflammation-swelling, warmth, redness around the joint
- You’ve tried injections but can’t keep getting them due to limited annual limits
- You’re not a candidate for surgery or want to delay it
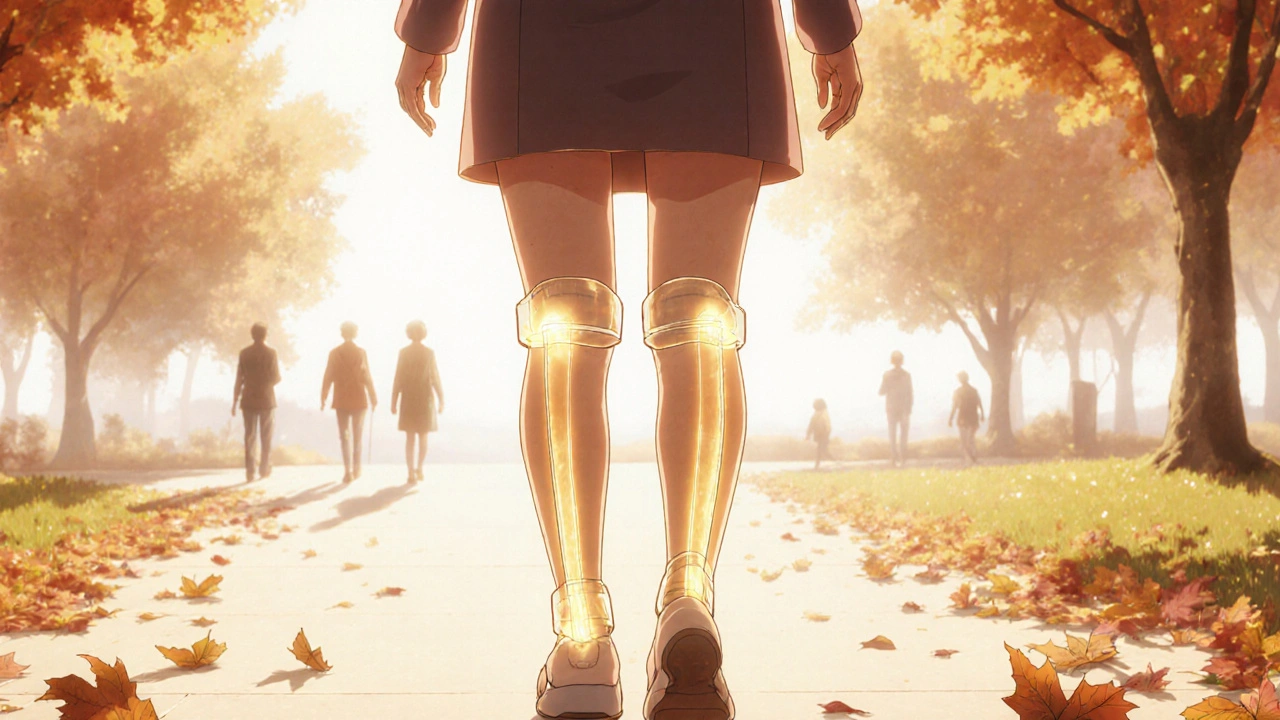
It’s especially useful for people over 60 with multiple joint involvement. A 2023 observational study from São Paulo followed 87 patients with knee and hip osteoarthritis on low-dose deflazacort. After one year, 68% reported being able to walk without a cane, and 54% reduced their use of opioids.
The Risks: What No One Tells You
Here’s the catch: corticosteroids aren’t harmless. Even at low doses, long-term use can cause problems.
Common side effects include:
- Increased appetite and weight gain
- Mood swings or trouble sleeping
- Higher blood sugar levels-dangerous if you have prediabetes
- Thinner skin and easier bruising
- Increased risk of infections
Long-term use (over 6 months) can lead to osteoporosis, cataracts, or adrenal suppression. That’s why doctors rarely prescribe it for more than 3 to 6 months at a time. It’s not a cure. It’s a tool to get you through a flare-up.
People with glaucoma, active infections, or a history of peptic ulcers should avoid it. If you’re on blood thinners or diabetes meds, your doses may need adjusting.
How It Fits Into a Real Treatment Plan
Deflazacort doesn’t replace physical therapy or weight loss. It complements them.
A typical approach looks like this:
- Start with non-drug treatments: walking, water exercises, knee braces, heat packs
- If pain persists after 6 weeks, try NSAIDs like ibuprofen or naproxen
- If those fail or cause stomach issues, consider a short course of deflazacort (4-12 weeks)
- During treatment, monitor blood pressure, blood sugar, and bone density
- After stopping, ramp up physical therapy to rebuild strength and prevent relapse
Some clinics in Australia and Brazil now use it as a bridge to surgery-helping patients regain enough function to tolerate rehab after a joint replacement.
Alternatives to Consider
If deflazacort feels too risky, here are other options:
| Treatment | Effectiveness | Duration of Relief | Main Risks |
|---|---|---|---|
| Deflazacort (oral) | High for inflammatory OA | 2-6 months | Weight gain, high blood sugar, bone loss |
| Prednisone (oral) | High | 1-4 months | More muscle wasting, higher infection risk |
| Joint injections (cortisone) | Moderate to high | 3-6 weeks per shot | Cartilage damage with frequent use |
| NSAIDs (e.g., naproxen) | Moderate | Hours to days | Stomach ulcers, kidney strain |
| Physical therapy + weight loss | Moderate to high | Long-term, if maintained | Low |
For many, a combination of physical therapy and one or two cortisone shots works better than long-term pills. But if you’ve hit the limit on injections and can’t tolerate NSAIDs, deflazacort becomes a realistic option.

What Doctors Say About It
Most rheumatologists in Australia still see deflazacort as a second-line option. But attitudes are shifting.
Dr. Helen Lin, a rheumatologist at Royal North Shore Hospital in Sydney, says: “We used to avoid steroids in osteoarthritis unless it was a flare tied to another condition. But now, with better monitoring and shorter courses, we’re seeing real benefits in patients who’ve run out of options. It’s not for everyone-but it’s not for no one either.”
She recommends starting at the lowest effective dose (6 mg/day) and checking in every 4 weeks. Blood tests for glucose and electrolytes are standard. Bone density scans are advised if treatment goes beyond 3 months.
When to Stop Taking It
You don’t quit deflazacort cold turkey. Stopping suddenly can trigger adrenal insufficiency-your body forgets how to make its own cortisol.
Always taper down slowly. A typical plan:
- Week 1-2: Reduce by 3 mg every 5 days
- Week 3-4: Reduce by 1.5 mg every 5 days
- Stop when you reach 3 mg or lower
Your doctor should guide this. If you feel dizzy, nauseous, or extremely tired during tapering, call your provider. It might mean you need to slow down.
Final Thoughts
Deflazacort isn’t a miracle drug for osteoarthritis. But for some, it’s the difference between staying active and staying home. It’s not about avoiding pain-it’s about reclaiming movement. If you’ve tried everything else and your joints still scream, talk to your doctor about whether a short, controlled course of deflazacort could be part of your plan.
It’s not about taking pills forever. It’s about giving your body a break so you can rebuild-through movement, through strength, through time.
Can deflazacort cure osteoarthritis?
No, deflazacort cannot cure osteoarthritis. It reduces inflammation and eases symptoms, but it doesn’t repair damaged cartilage or stop the disease from progressing. It’s a symptom manager, not a disease modifier.
Is deflazacort approved for osteoarthritis in Australia?
Deflazacort is not specifically approved by the TGA for osteoarthritis, but it is approved for other inflammatory conditions. Doctors can prescribe it off-label if they believe the benefits outweigh the risks. Many patients in Australia get it through private prescriptions or import programs.
How long does it take for deflazacort to work for joint pain?
Most people notice reduced swelling and pain within 7 to 14 days. Full effects usually appear by 4 weeks. If you don’t feel any change after 6 weeks, it’s unlikely to help you-your doctor may suggest another option.
Can I take deflazacort with other arthritis meds?
You can take it with most pain relievers like acetaminophen, but avoid combining it with NSAIDs unless your doctor approves it. Mixing steroids and NSAIDs increases the risk of stomach ulcers. Also, never take it with live vaccines or certain antifungals like ketoconazole.
What happens if I miss a dose of deflazacort?
If you miss a dose, take it as soon as you remember. But if it’s close to your next scheduled dose, skip the missed one. Never double up. Missing doses occasionally won’t cause major issues, but inconsistent use can make inflammation rebound.
Are there natural alternatives to deflazacort for osteoarthritis?
Some people find relief with omega-3 fatty acids, turmeric (curcumin), or glucosamine, but studies show these help only mildly-especially for moderate to severe pain. They’re good for prevention or mild cases, but not substitutes for anti-inflammatory steroids when inflammation is active and debilitating.
Will deflazacort make me gain weight?
Yes, weight gain is common, especially around the face, abdomen, and back. This is due to fluid retention and increased appetite. Eating a low-sodium, high-protein diet and staying active can help minimize it. Most of the weight comes off after you stop the medication.

13 Comments
Ankit Yadav
3 November, 2025Been on deflazacort for 5 months now for knee OA. No more cane. No more opioid nights. Weight gain? Yeah. Face mooning? Totally. But I can play with my grandkids again. That’s worth it. Tapering slow like the doc said-no drama.
Meghan Rose
4 November, 2025Wait so you’re just gonna take steroids for joint pain? Like… isn’t that what got your friend’s bones to turn to dust? I’m just saying. I saw a documentary.
Steve Phillips
4 November, 2025Ohhhhh, so you’re telling me that a glorified prednisone knockoff-*with a slightly less catastrophic side effect profile*-is now the *hero* of OA management? How utterly *dramatic*. The sheer *audacity* of this article to suggest that a synthetic glucocorticoid is anything but a temporary bandage on a crumbling cathedral of cartilage! I mean, have you SEEN the bone density curves? The adrenal suppression? The *dramatic* weight gain that turns people into walking marshmallows? This isn’t medicine-it’s a slow-motion tragedy with a 6-month expiration date. And yet… here we are. We’re all just… waiting for the next flare.
Rachel Puno
6 November, 2025If you’re thinking about this, please talk to your PT first. Movement is the real medicine. Deflazacort might give you breathing room, but it won’t rebuild your strength. Don’t skip the squats just because the pills help. You got this 💪
Clyde Verdin Jr
6 November, 2025So let me get this straight… you’re recommending we poison our bodies with a steroid that makes us fat, sleepy, and diabetic… just so we can walk without crying? 🤡 I mean, come ON. This is like replacing your car’s engine with a lit firecracker. Sure it moves… but at what cost?? Also, who wrote this? A pharma rep with a thesaurus? 😭
Key Davis
7 November, 2025It is imperative to underscore that the off-label utilization of deflazacort for osteoarthritic pathology must be undertaken only under the direct supervision of a qualified rheumatological practitioner. The pharmacokinetic profile, while favorable relative to prednisone, remains subject to significant metabolic perturbations, particularly in elderly cohorts with comorbid metabolic syndrome. Furthermore, the potential for iatrogenic adrenal suppression necessitates rigorous longitudinal monitoring, including morning cortisol levels and bone mineral density assessments. To suggest this as a routine intervention is, in my professional estimation, both premature and potentially hazardous.
Cris Ceceris
8 November, 2025I wonder if we’re treating the symptom because we’re afraid of the cause. Osteoarthritis isn’t just ‘wear and tear’-it’s inflammation, sure, but why is the body doing that? Is it diet? Stress? Lack of sleep? Maybe deflazacort gives us back mobility, but what if the real fix is quieter? Less chemical, more… human? I’m not saying no to the pill, but I’m asking: are we just putting a bandaid on a wound we refuse to look at?
Brad Seymour
8 November, 2025Interesting take. I’ve seen this work in my physio clinic-old folks come in barely able to stand, on deflazacort for 8 weeks, and suddenly they’re doing water aerobics like it’s nothing. Not a miracle, but a damn good bridge. Just don’t forget to move when the pills stop.
Malia Blom
8 November, 2025Oh so now we’re just gonna hand out corticosteroids like candy because we’re too lazy to fix the real problem? You know what else reduces inflammation? Not eating processed food. Not sitting on your ass all day. Not ignoring your mental health. But nooo, let’s just pop a pill and call it a day. Classic American medicine. Fix the symptom, ignore the system. Also, who even uses deflazacort? Is this even legal here? I feel like this is a Brazilian pharmacy hack.
Erika Puhan
10 November, 2025Deflazacort? Are you kidding me? The pharmacokinetic half-life is misleadingly optimized for compliance, yet the systemic immunosuppressive burden-particularly IL-6 and TNF-alpha modulation-is catastrophically underreported in low-dose OA protocols. The bone turnover markers in the São Paulo cohort? They didn’t even adjust for baseline vitamin D deficiency. This is pseudoscience dressed in clinical jargon. And the ‘68% improved’ stat? That’s self-reported. No objective gait analysis. No MRI correlation. Pathetic.
Edward Weaver
11 November, 2025Why are we letting foreign drugs dictate our treatment? Prednisone is American. Deflazacort? Made in India. Brazil. Who even approved this? We’ve got the best doctors here. Why are we importing pills from countries where they don’t even have proper health insurance? This is cultural surrender. And don’t get me started on the weight gain-Americans already struggle enough with obesity. This is just giving people a chemical excuse to quit.
Lexi Brinkley
11 November, 2025So… I tried this. 😅 I gained 12 lbs in 2 months. My face looks like a balloon. But I can finally pick up my dog again 🐶❤️ So… worth it? Maybe. My doc says I’m doing great. But I miss my old jeans. 😭
Kelsey Veg
12 November, 2025deflazacort?? like… is that even a word? i thought it was deflazacort or something? i mean i googled it and it looks real but why does it sound like a brand of energy drink? also i took it for 2 weeks and my butt hurt more??