Herbal and supplement liver toxicity is real - and it’s rising fast
People turn to herbal supplements for energy, weight loss, or better sleep. They think ‘natural’ means safe. But the truth? Many of these products are quietly damaging the liver - sometimes without warning. In Australia, the U.S., and across the globe, hospital admissions for liver injury caused by supplements have more than doubled in the last 15 years. The liver doesn’t scream when it’s under attack. By the time symptoms show up, it’s often too late.
These six supplements are the most dangerous for your liver
Research from 2024, published in JAMA Network Open, analyzed thousands of cases and found six botanicals linked to the most severe liver damage. These aren’t obscure herbs - they’re everywhere. You’ll find them in teas, capsules, powders, and TikTok-endorsed ‘super blends’.
- Turmeric or curcumin: Often sold as an anti-inflammatory, high-dose turmeric supplements have caused acute hepatitis. One study found patients taking 1,000 mg or more daily for months developed liver enzyme spikes - even if they had no prior liver issues.
- Green tea extract: It’s not the tea you drink. It’s the concentrated pills. EGCG, the active compound, can overload liver cells. Consumer Reports found 25% of green tea extract products exceeded safe daily limits. Some users developed liver failure after just 6-8 weeks.
- Garcinia cambogia: Marketed for weight loss, this fruit extract has been tied to liver inflammation and jaundice. In one U.S. case series, 14 patients were hospitalized after using weight-loss products containing it.
- Black cohosh: Commonly used for menopause symptoms, this herb has caused acute liver injury in multiple documented cases. The NIH’s LiverTox database lists over 50 reports of liver damage linked to black cohosh.
- Red yeast rice: Sold as a ‘natural statin,’ it contains monacolin K - the same compound as the prescription drug lovastatin. But without dosage control, it can cause rhabdomyolysis and liver stress. Many products are also contaminated with citrinin, a toxic mold byproduct.
- Ashwagandha: Popular for stress and sleep, ashwagandha has been flagged in recent studies for causing elevated liver enzymes. Cases are rare, but they’re consistent enough that doctors now ask about it during liver evaluations.
What’s really in your supplement bottle?
Here’s the scary part: what’s on the label isn’t always what’s inside. A 2017 study found that up to 60% of herbal supplements are mislabeled or adulterated. You might think you’re taking pure turmeric. Instead, you’re getting turmeric mixed with undisclosed pharmaceuticals, heavy metals, or pesticides.
The FDA doesn’t test supplements before they hit shelves. That means:
- 18% of tested products contained lead - enough to trigger warnings under California’s Prop 65.
- 22% of sexual enhancement supplements had sildenafil (Viagra) hidden inside.
- 15% of pain relief supplements had NSAIDs like ibuprofen added without disclosure.
- 23% of herbal products had pesticide residues.
- 7% were contaminated with bacteria or fungi.
These aren’t outliers. They’re standard. A 2023 Consumer Reports test of 20 turmeric supplements found 30% had lead levels above safety limits. And lead doesn’t just hurt your brain - it builds up in your liver, causing chronic inflammation and scarring over time.

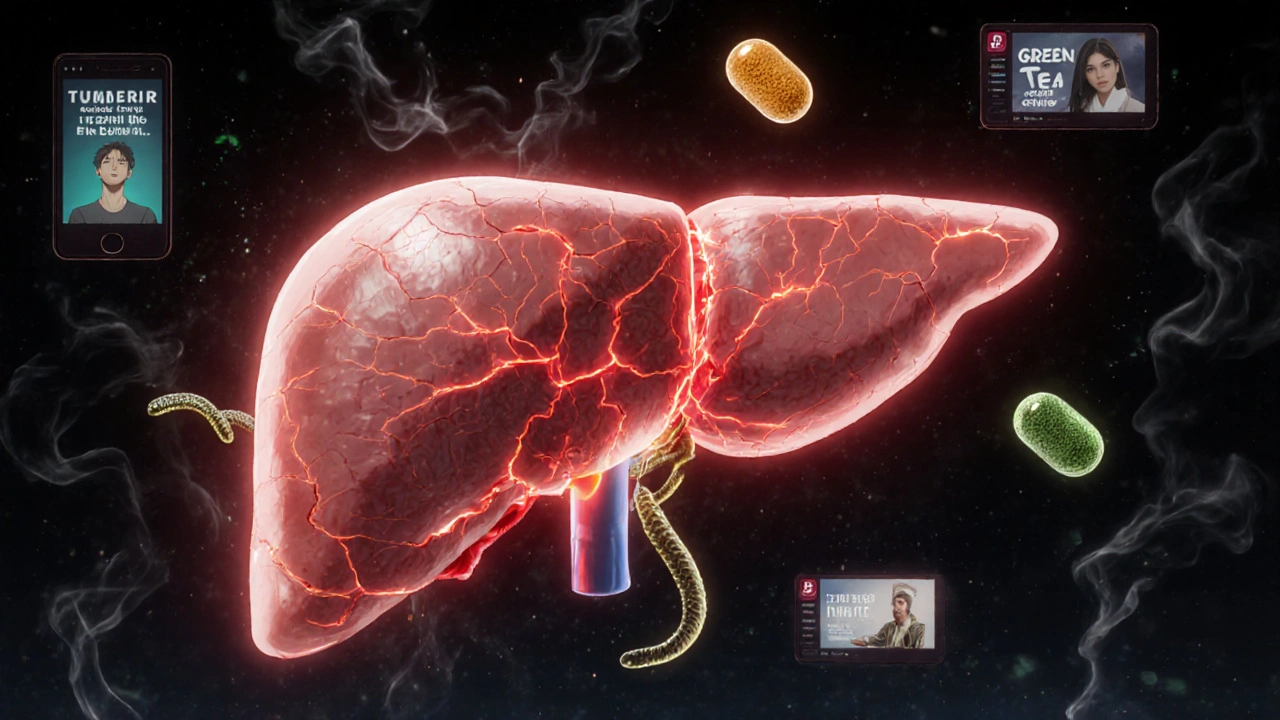
Why your liver can’t handle these products
Your liver is your body’s main detox center. It breaks down everything you take - food, alcohol, medications, supplements. But herbs and botanicals? They’re complex chemical mixtures. Your liver has to process dozens of unknown compounds at once, many with no safety data.
Unlike prescription drugs, supplements don’t go through clinical trials. No one tested how 500 mg of ashwagandha affects someone with a slow-metabolizing CYP3A4 gene variant. No one checked if green tea extract interacts with your thyroid medication. That’s the gap.
Dr. Robert S. Brown from Weill Cornell Medicine puts it simply: ‘It’s like an allergy. A small amount of a toxin can destroy the liver in some people - even if it’s harmless to others.’
Some people have genetic differences that make them more vulnerable. Research suggests the HLA-B*35:01 gene variant increases risk for certain herbal liver injuries. But no one screens for this. You won’t know you’re at risk until your liver fails.
Signs your liver is under attack
Most people don’t feel anything until it’s serious. But there are early red flags - and they’re often ignored.
- Fatigue (87% of cases)
- Abdominal pain (76%) - usually in the upper right side
- Nausea or vomiting (68%)
- Dark urine (52%) - like cola or tea
- Yellow skin or eyes (jaundice)
- Itchy skin
- Unexplained weight loss
If you’ve been taking any of these supplements and notice even one of these symptoms, stop immediately. Get a liver function test. Don’t wait. Many patients only find out they have liver damage after being hospitalized for acute failure.
Who’s most at risk?
It’s not just the elderly or people with existing liver disease. The fastest-growing group of cases? Young adults - especially those under 35.
Social media is driving this. TikTok influencers push ‘clean’ weight-loss teas, detox powders, and ‘natural’ testosterone boosters. They don’t mention liver risks. They don’t mention that the ‘organic’ ashwagandha they’re using might have lead in it. They don’t mention that ‘natural’ doesn’t mean safe.
Women using black cohosh for menopause. Men taking red yeast rice to lower cholesterol. Students using green tea extract for focus. Athletes loading up on turmeric for recovery. All are at risk.
And here’s the kicker: the liver can heal - if you catch it early. But if you keep taking the supplement, damage becomes permanent. Cirrhosis. Transplant. Death.
What you can do right now
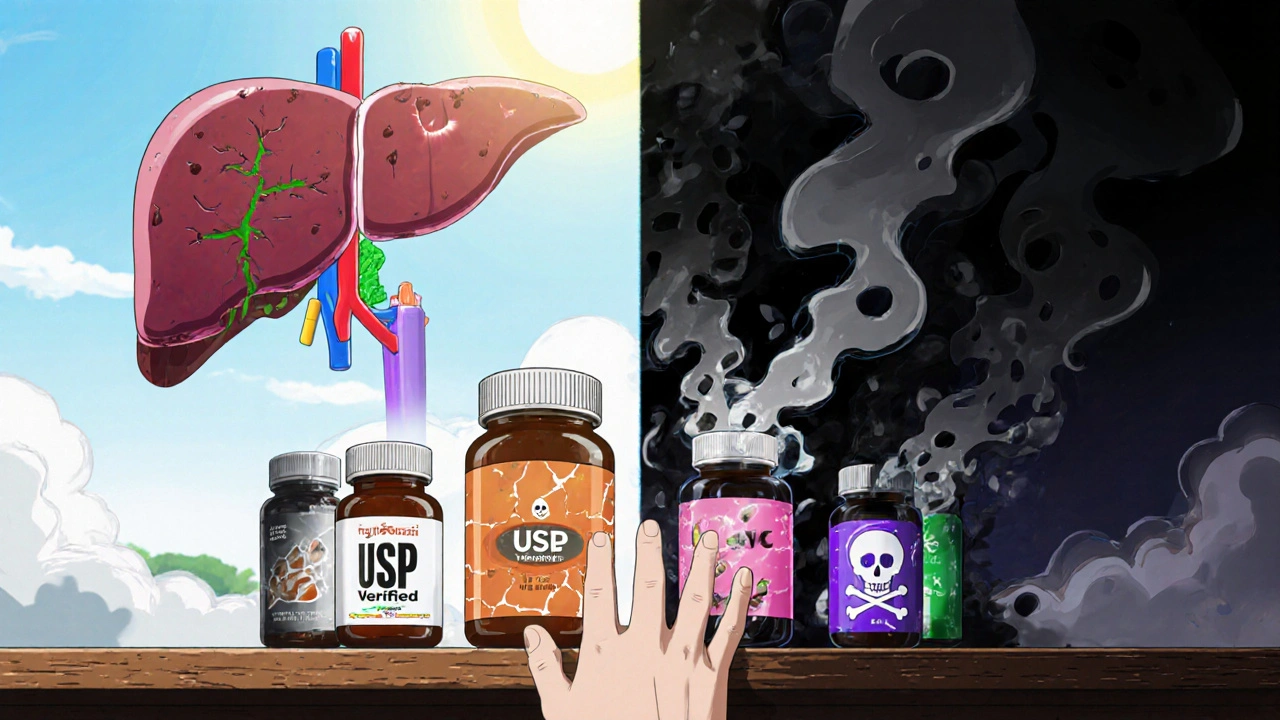
You don’t need to avoid all supplements. But you need to be smarter.
- Stop taking high-dose extracts. If it says ‘500 mg extract’ or ‘concentrated,’ put it down. Whole herbs are safer than extracts - but still not risk-free.
- Check for third-party testing. Look for seals from USP, NSF, or ConsumerLab. These don’t guarantee safety, but they do verify what’s on the label.
- Never combine supplements. Taking turmeric + ashwagandha + green tea extract? That’s a recipe for liver overload. One is risky. Three? Deadly.
- Talk to your doctor. Tell them every supplement you take - even if you think it’s ‘just herbal.’ They need to know when your ALT or AST levels are high.
- Don’t trust TikTok or Instagram. If an influencer says ‘this tea cleanses your liver,’ they’re wrong. Your liver cleanses itself. No tea can do that.
The bottom line
Herbal supplements aren’t regulated like medicine. That’s not a bug - it’s the system. And it’s putting lives at risk. The liver doesn’t have a warning light. It doesn’t beep when it’s failing. It just stops working - quietly.
If you’re taking any of the six high-risk herbs listed here, stop. Get tested. Talk to a doctor. And next time you’re tempted by a ‘miracle’ supplement, ask: who tested this? Who knows what’s inside? And who’s going to pay for the damage?
Can herbal supplements cause permanent liver damage?
Yes. If liver injury from supplements goes undetected and continues over time, it can lead to fibrosis, cirrhosis, or even acute liver failure requiring a transplant. Many patients recover fully if they stop the supplement early - but others are left with lasting damage. The key is early detection.
Are ‘organic’ or ‘natural’ supplements safer?
No. ‘Organic’ only means the plants were grown without synthetic pesticides - it says nothing about purity, dosage, or contamination. Many organic supplements still contain heavy metals, undisclosed drugs, or toxic mold. Natural doesn’t equal safe.
Why doesn’t the FDA ban these dangerous supplements?
Under the Dietary Supplement Health and Education Act (DSHEA) of 1994, the FDA can’t remove a supplement from the market unless it proves it’s unsafe after people are already harmed. That means thousands of people get injured before regulators can act. The burden of proof is on the FDA - not the manufacturer.
Is green tea safe if I drink it as a beverage?
Yes. Drinking 2-3 cups of green tea per day is generally safe. The danger comes from concentrated extracts in pills or powders, which deliver 10-100 times more EGCG than tea. That’s what overwhelms the liver. Stick to tea, not capsules.
Should I get my liver tested if I take supplements?
If you’ve been taking herbal supplements for more than 3 months - especially turmeric, green tea extract, or black cohosh - yes. A simple blood test for ALT and AST can catch early liver damage before symptoms appear. The American College of Gastroenterology recommends this for anyone with unexplained liver enzyme elevations.
What’s the safest way to support liver health?
The liver heals best with rest - not more supplements. Avoid alcohol, processed foods, and excess sugar. Eat vegetables, stay hydrated, and maintain a healthy weight. Exercise helps. Sleep helps. The best liver detox is doing nothing but giving your body time to recover.

10 Comments
David vaughan
20 November, 2025I started taking turmeric for my knees last year... never thought about liver damage. Just stopped it after reading this. Got my ALT checked last week - it's back to normal. Seriously, folks, don't ignore fatigue or dark urine. It's not just 'being tired'.
Thanks for posting this.
Logan Romine
21 November, 2025So let me get this straight... we're told 'natural = safe' by influencers who get paid to sell us snake oil, then we're shocked when our livers give up? 🤡
Meanwhile, Big Pharma gets fined $200M for a single side effect. But a guy on TikTok selling 'detox tea' with lead and undisclosed Viagra? That's just 'free speech' and 'personal choice'.
Capitalism is a horror show.
Mark Kahn
22 November, 2025This is so important. My cousin was hospitalized last year after using a 'natural testosterone booster' from Amazon. Turned out it had hidden sildenafil AND a heavy metal cocktail. He's fine now, but it took 3 months. Please, if you're taking anything labeled 'miracle' or 'ancient secret' - just don't.
Steve Harris
23 November, 2025I'm a nurse in a GI unit. We see this every month. Young guy, 28, no history of drinking, no obesity - comes in with jaundice and ALT over 2000. Asks if it's 'maybe the green tea pills'. We pull the bottle - yeah, it's the 1000mg extract. He thought 'more is better'. It's not. It's a death sentence with a wellness brand on it.
Stop trusting influencers. Start trusting labs.
Shawn Sakura
24 November, 2025i just found out my ashwagandha had lead in it?? i thought organic meant safe 😭 i stopped it last week and i feel way better already. my doctor said my enzymes were creeping up. thanks for the heads up. i’m gonna get tested next week. 🙏
Cooper Long
26 November, 2025The regulatory failure here is systemic. DSHEA was designed to protect small herbal vendors from overreach - not to enable mass poisoning under the banner of 'freedom'. The FDA lacks funding, authority, and political will. Until supplement manufacturers are held to the same standard as pharmaceuticals, this will continue. This is not a consumer education problem. It is a policy failure.
Chris Vere
27 November, 2025In Nigeria we don't have much access to these supplements but when they come in, people buy them like they are holy water. No testing. No labels. Just a bottle with a picture of a tree and the word 'pure'. I told my cousin to stop her 'weight loss tea' - she said 'it's natural, how can it hurt?'. I just shook my head. The liver doesn't care if it's organic or not. It just wants to live.
Pravin Manani
27 November, 2025From a pharmacogenomics standpoint, the HLA-B*35:01 variant is a critical risk factor for herb-induced liver injury, particularly with black cohosh and green tea extract. Most clinicians don't screen for it because it's not cost-effective - but if you have unexplained transaminitis and a history of botanical use, genetic testing should be considered. Also, CYP3A4 polymorphisms dramatically alter metabolite clearance. This isn't 'luck' - it's biochemistry.
Michael Marrale
28 November, 2025I’ve been saying this for years. The FDA is in bed with Big Herbal. They know. They’ve known since 2010. The real reason they don’t ban these is because the same people who run the supplement companies also donate to Congress. And the CDC? They’re too busy telling people to drink more water. This is a cover-up. The liver isn’t failing - it’s being murdered by corporate greed. Wake up.
Leo Tamisch
28 November, 2025Ah yes. The classic 'just stop taking supplements' advice. As if we’re all sitting around with a spreadsheet of every phytochemical we ingest. Meanwhile, the real solution is to stop pretending the body needs 'detox' - it’s a self-cleaning oven. But hey, if selling fear and 'miracle powders' makes you $500M/year, who cares if 0.1% of users get liver failure? It’s just business. 🤷♂️