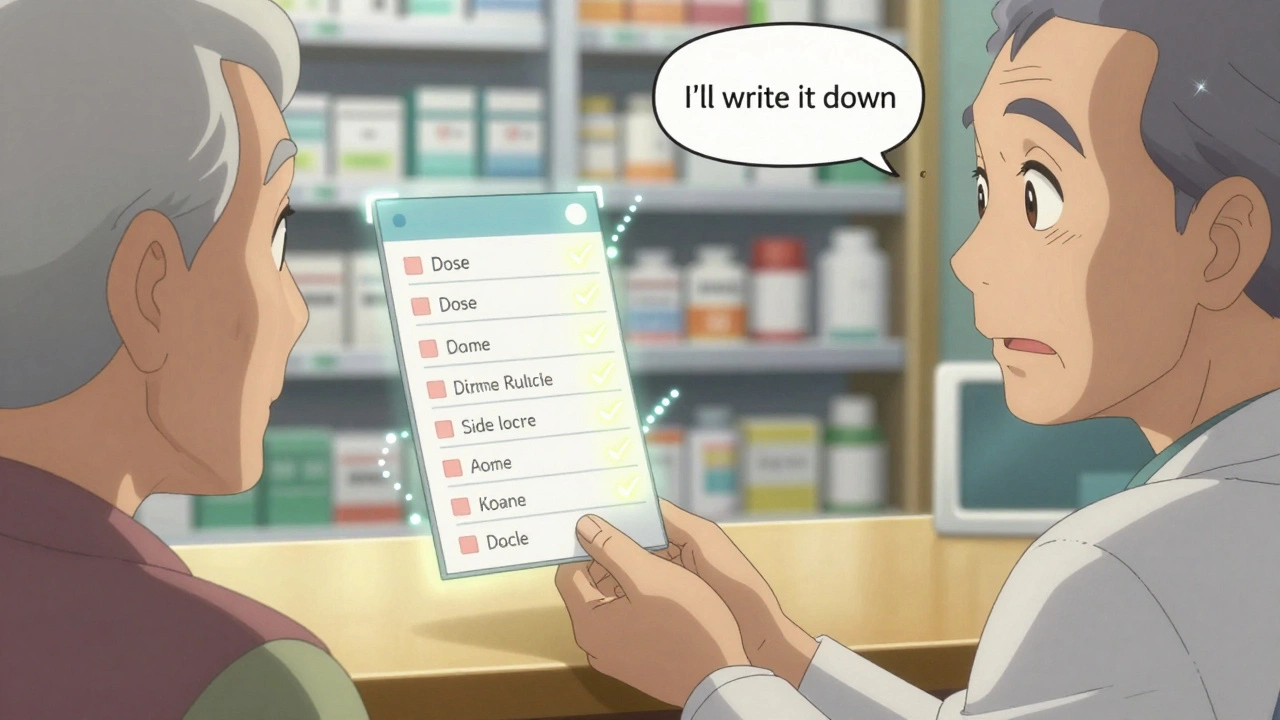
When your doctor or pharmacist gives you advice about your medications, it’s easy to think, "I’ll remember this." But by the time you get home, juggling kids, work, or just plain fatigue, details blur. Did they say take it with food or on an empty stomach? Was the dose 10 mg or 20 mg? Did they warn you about dizziness or a bad reaction with alcohol? Writing it down isn’t just a good habit-it’s a safety net.
Why Documentation Matters More Than You Think
Medication errors cause about 7,000 deaths in the U.S. every year, according to the Institute of Medicine. A lot of those happen because information gets lost between visits, pharmacies, or even within your own memory. When you document what your provider tells you, you’re not just helping yourself-you’re helping every other provider who might treat you later. Emergency rooms, pharmacists, specialists-they all need to know exactly what you’re taking and why.What Exactly Should You Write Down?
Don’t just scribble "take pill twice a day." Be specific. Here’s what to include for every medication:- Medication name - Both brand and generic if given (e.g., "Lisinopril (Zestril)")
- Dose - Exact amount (e.g., "10 mg", not "one pill")
- Frequency - "Take once daily at bedtime" or "every 8 hours as needed for pain"
- Duration - "Take for 14 days" or "refills: 3"
- Special instructions - "Take with food," "avoid grapefruit," "do not crush," "shake well before use"
- Purpose - "For high blood pressure," "for infection," "for anxiety"
- Side effects to watch for - "If you feel dizzy or swollen ankles, call the office"
- What to do if you miss a dose - "Skip it if it’s almost time for the next dose"
- Allergies or reactions - Even if you already told them, write it again: "Allergic to penicillin-rash and swelling"
Also note any advice about non-medication things: "Avoid alcohol while on this," "Check blood pressure weekly," "Call if fever lasts more than 48 hours." These details matter.
How to Document It - The Right Way
You don’t need fancy tools. A notebook, a notes app, or even your phone’s voice recorder works. But here’s how to make it useful:- Date and time every entry - Write the date you spoke with the provider. If you’re unsure, write "as of Dec 3, 2025".
- Write the provider’s name and role - "Dr. Chen, PCP" or "Pharmacist Rivera, Walgreens"
- Use your own words - Don’t copy what they said word-for-word unless it’s critical. Summarize clearly. "They said: don’t take with milk. I wrote: avoid dairy for 2 hours after taking this pill."
- Record refusals or confusion - If you didn’t understand, write that too. "Didn’t understand why I need this med. Asked for written info."
- Save receipts or printed sheets - Many pharmacies give you a printed label with instructions. Tape it into your notebook or take a photo.
Some people use apps like Medisafe or MyTherapy. They’re helpful, but they’re not foolproof. Always double-check what’s in the app against what your provider said. Apps can glitch. Your handwritten note won’t.
What Providers Are Required to Document (And Why You Should Too)
Healthcare systems are legally required to document medication advice. The Joint Commission, CMS, and the American Medical Association all say: if it wasn’t written down, it didn’t happen. That’s not just bureaucracy-it’s protection.Providers must record:
- Medication changes at every visit
- Education given about side effects or interactions
- Refusals to take meds or follow advice
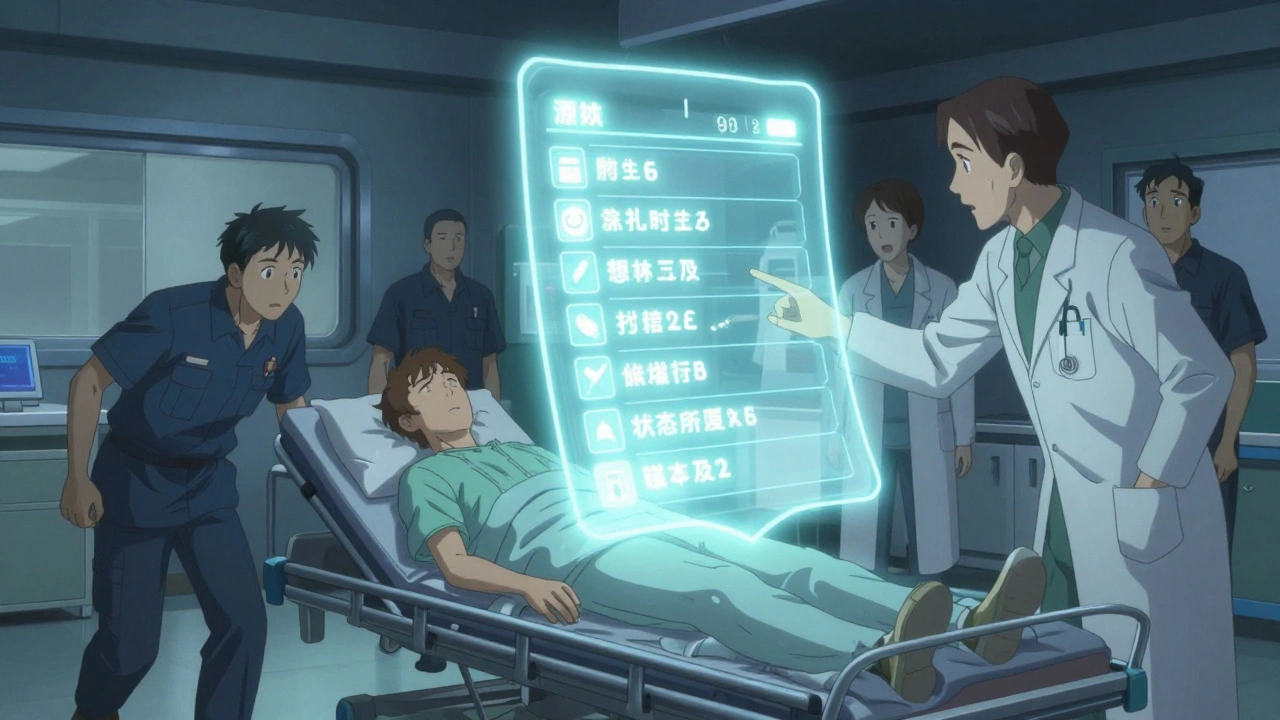
- Medication reconciliation at every transition of care (e.g., hospital to home)
But here’s the catch: providers are busy. They might forget to write down everything they told you. That’s why your personal record is just as important as theirs. If you’re ever in a situation where your care is questioned-like an ER visit or a malpractice review-your documentation can be the difference between clarity and chaos.
Electronic Health Records Aren’t Enough
About 89% of doctors now use electronic health records (EHRs), and by 2025, nearly all medication documentation will happen digitally. That sounds great, right? But EHRs aren’t perfect. They’re often cluttered, hard to navigate, and not always shared between systems. Your grandma’s cardiologist might not see what your dermatologist wrote. Your pharmacy might not get the update.Even if your provider uses a patient portal, you can’t assume everything’s there. Some instructions are buried in notes only providers can read. Some changes aren’t synced right away. Your personal record acts as your backup copy.
What to Do When You Don’t Understand
If your provider says something confusing, don’t nod and smile. Say: "Can you repeat that?" or "Can you write it down?"It’s your right to understand. If they brush you off, ask for a pharmacist to explain it. Most clinics have one on staff. If you’re still unsure, call back. Say: "I need clarification on my medication instructions. Can you send me a written summary?"
Some pharmacies now offer free medication counseling. Use it. Write down what they say. Keep it with your other notes.
Keep It Organized and Accessible
Don’t let your notes pile up in random places. Create one simple system:- Use a binder or notebook labeled "My Medications"
- Divide by medication or by date
- Keep a list of all current meds at the front
- Take a photo of the page and save it in your phone’s cloud storage
- Give a copy to a trusted family member or caregiver
If you’re managing multiple meds, make a chart. One column for the name, one for dose, one for time of day, one for notes. Update it every time something changes.
When to Review and Update
Don’t set it and forget it. Review your medication notes:- Before every doctor visit
- After every pharmacy refill
- After any hospital stay or ER visit
- Every 3 months, even if nothing changed
Ask yourself: "Is this still right?" Did you stop a med? Did they change the dose? Did you start a new one? Update your notes immediately.
Legal and Safety Consequences of Poor Documentation
Inadequate documentation contributes to 22% of preventable adverse drug events in outpatient care, according to the National Committee for Quality Assurance. And in malpractice cases, 38% involve medication errors.Imagine this: You’re in the ER after a fall. You’re confused. You can’t remember your meds. The doctors don’t know if you’re on blood thinners, insulin, or heart meds. They give you a drug that interacts dangerously. That’s not hypothetical. It happens every day.
Your documentation isn’t just helpful-it’s life-saving. It’s also your legal protection. If you’re ever accused of noncompliance, your notes prove you were trying.
What’s Coming Next
Starting in 2025, the FDA is pushing for a standardized one-page patient medication info sheet (PMI) to come with every new prescription. This will include clear instructions, side effects, and warnings in plain language. It’s a big step forward.But until then, you still need to document. Even with PMI, your provider might add extra advice that doesn’t appear on the sheet. Your personal record fills those gaps.
Final Tip: Make It a Habit
The best documentation system is the one you actually use. Pick a method-paper, phone, app-and stick with it. Don’t wait until you’re confused or in crisis. Start today.After your next appointment, take five minutes. Write down what was said. Date it. Sign it. Keep it safe. That small step could prevent a hospital visit, a bad reaction, or worse.
What if I forget to write down what my doctor said?
Call the office or pharmacy within 24 hours. Ask them to email or mail you a written summary. Most providers will do this if you ask. Don’t wait-details fade fast.
Can I use my phone’s voice recorder instead of writing?
Yes, but only if you transcribe it later. Voice recordings are hard to search and can be lost if your phone dies or gets replaced. Write down the key points right after the call. Use the recording as backup, not your main system.
Do I need to document advice from nurses or pharmacists too?
Absolutely. Nurses and pharmacists often give the most detailed instructions on how to take meds safely. Record their names and what they said just like you would for your doctor. Their advice is just as important.
How long should I keep my medication records?
Keep them for at least 7 years, especially for chronic conditions. Some states require records to be kept 10 years. Even after you stop a medication, keep notes on why it was prescribed and when you stopped. This helps future providers understand your medical history.
What if I’m not comfortable writing things down?
Try using a voice-to-text app on your phone. Say your notes out loud while you’re still in the car after your appointment. Then copy the text into a notes app or email it to yourself. The goal isn’t handwriting-it’s capturing the information reliably.
Should I bring my notes to every appointment?
Yes. Bring your medication log to every visit. It helps your provider spot errors, track changes, and avoid prescribing something that conflicts. It also shows you’re engaged in your care-which improves outcomes.
Documenting medication advice isn’t a chore-it’s your power tool for safer, smarter health care. Do it consistently, and you’ll never have to guess what you were told again.


16 Comments
sean whitfield
5 December, 2025The system is rigged. They want you to write everything down so they can sell your data to Big Pharma. I don't trust doctors. I don't trust pharmacies. I don't trust apps. I trust my gut and a handwritten note on a napkin. That's the only real record.
They say 'document for safety.' I say: document so they can track you.
Next they'll make you sign a waiver every time you breathe.
Wake up.
They're not helping you. They're harvesting you.
Jennifer Patrician
5 December, 2025Oh please. You think writing stuff down is going to save you from the pharmaceutical-industrial complex? You're just doing their job for free. They get paid to give you advice. You get punished if you forget. That's not safety. That's control. And now you're proud of being a compliance robot?
My grandma took her meds by smell. She lived to 98. No notes. No apps. Just instinct. You think she was dumb? She was wise.
Stop feeding the machine.
aditya dixit
7 December, 2025This is one of those rare posts that actually helps. I've seen too many patients in rural India come in with half-remembered instructions, confused about dosages, terrified of side effects they misunderstood.
Documentation isn't bureaucracy - it's dignity.
When someone is ill, their mind is already overloaded. Memory is unreliable. Emotions cloud judgment. Writing it down isn't a chore - it's an act of self-respect.
And yes, even if your provider is busy, your note becomes their backup. It bridges gaps in a broken system.
Start small. One medication. One note. One date. That's how change begins.
You're not just recording pills. You're recording your right to be heard.
Norene Fulwiler
8 December, 2025I'm a nurse and I see this every day. A woman comes in after a fall, can't remember her blood thinner, and the ER team almost gives her ibuprofen - which would've caused a bleed. She had the list in her purse. Just didn't think to pull it out.
So I told her: next time, tape it to your fridge. Or put it in your phone's lock screen.
It's not about being perfect. It's about being visible.
Your life doesn't live in your head. It lives in your habits.
Make this one habit stick.
William Chin
9 December, 2025It is imperative that individuals assume full responsibility for the accurate documentation of pharmaceutical directives issued by licensed healthcare professionals. Failure to do so constitutes a dereliction of duty that endangers not only the individual, but the broader public health infrastructure. The Joint Commission mandates this for a reason: negligence is not an option.
Furthermore, the use of unregulated digital applications introduces unacceptable risk vectors. Paper documentation, securely stored in a fireproof container, remains the gold standard.
I urge all readers to immediately implement this protocol. Your life depends on it.
Deborah Jacobs
11 December, 2025I used to think this was extra work - until my mom had a stroke and couldn't tell them what meds she was on. They gave her something that made her heart race like a hummingbird on espresso. She was scared. We were terrified.
So now I write everything. In purple ink. On sticky notes. On my mirror. On my coffee mug. On my phone. On my grandma's old recipe box.
It's not pretty. It's not neat. But it's alive.
My mom's alive too. And I owe that to a stupid sticky note that said: "Don't mix with grapefruit. Ever. Not even once."
That note saved her. Not the doctor. Not the pharmacy. That stupid note.
Lucy Kavanagh
12 December, 2025Interesting. So now we're supposed to be personal medical clerks for a system that doesn't even share records between hospitals? And you're okay with that? We're not in the UK anymore, you know. Here, if you're not white, middle-class, and fluent in medical jargon, you're invisible.
My cousin got misdiagnosed because her notes weren't in the system. They assumed she was 'non-compliant.' She didn't even speak English well.
Documentation isn't the solution. It's the trap.
Fix the system. Don't make the patient fix it for you.
Chris Brown
13 December, 2025This is the kind of advice that makes me sick. You're telling people to document their own care like they're interns in a hospital? Where is the accountability? Where is the provider's responsibility? Why is the burden of memory, organization, and recall placed entirely on the sick, the elderly, the exhausted? This isn't empowerment. It's exploitation dressed up as self-help.
My grandfather died because his doctor forgot to document a drug interaction. Now we're supposed to write it down ourselves? No. We're supposed to sue.
Stop normalizing negligence.
Stephanie Fiero
14 December, 2025OMG YES. I started doing this after I mixed up my thyroid med and got panic attacks for a week. I wrote it on my hand with a Sharpie. Then I made a little card. Now I keep it in my wallet. My boyfriend says I'm obsessive. I say I'm alive.
Also - I typoed "Lisinopril" as "Lisinopril" like 3 times. I'm bad at spelling. But I got the dose right. That's what matters.
Don't let perfect be the enemy of done.
Just write something. Anything. Even if it's messy. Even if you hate it. Do it anyway.
Laura Saye
15 December, 2025There's a profound metaphysical dimension to this practice - the act of externalizing internal knowledge as a form of ontological anchoring. When we document our medication regimens, we are not merely recording pharmacological data; we are asserting our agency in a system that seeks to depersonalize the embodied experience of illness.
Each handwritten note becomes a sacrament of selfhood - a quiet rebellion against algorithmic governance and clinical abstraction.
It is not about compliance. It is about reclamation.
And in that reclamation, we find not just safety - but soul.
Michael Dioso
16 December, 2025You think this is new? I've been doing this since 2008. I've got a binder. Color-coded. Tabs. Index. QR code linking to my Google Drive. I even have a spreadsheet with side effect probabilities based on NIH data.
You're late to the game. And if you're using an app? You're already compromised. Most of them sell your data. I know because I checked the TOS. I'm not a moron.
Also - never trust a pharmacist who doesn't have a beard. It's a rule.
Krishan Patel
18 December, 2025Documenting medication advice is not optional - it is a moral imperative. In India, we say: 'A man who forgets his medicine is a man who forgets his life.'
Western culture has become so detached from responsibility that we outsource our survival to machines and bureaucrats.
You think your EHR is safe? It's not. It's a digital ghost. Your notebook? That's your soul on paper.
And if you can't write? Learn. If you can't read? Find someone who can. This is not a privilege. It is a duty to your ancestors and your descendants.
Carole Nkosi
18 December, 2025Documenting? That’s just the first step. Next they’ll make you record your dreams. Then your bowel movements. Then your emotional state before taking a pill. This is how they control you. They want you to become your own medical assistant so they don’t have to pay nurses.
I stopped taking all my meds. I’m fine. My body knows better than any doctor. The pills are poison. The system is poison. Write it all down? No. Burn it all down.
Ada Maklagina
19 December, 2025Just write it on your phone. No big deal. I use Notes. I type it while I'm still in the parking lot. Done.
My mom does it on a notepad. She's 82. She's fine.
Stop overthinking it.
Do the thing.
James Moore
20 December, 2025Let me be perfectly clear: the entire modern healthcare paradigm is a grotesque farce, engineered by pharmaceutical conglomerates and incentivized by profit-driven insurance intermediaries who have systematically dismantled the physician-patient relationship - replacing it with transactional, time-limited, algorithmically optimized encounters that prioritize efficiency over efficacy, compliance over comprehension, and documentation over dialogue.
And yet - we are told that the solution is for the patient, often elderly, often traumatized, often economically vulnerable - to become a paralegal of their own medical history?
It is not merely ironic - it is morally indefensible.
And yet - I document everything. Because I have no choice.
And I hate it.
And I’m not alone.
sean whitfield
22 December, 2025They're coming for the voice recorders next.
Next time you record your doctor, they'll say it's 'unauthorized.' Then they'll charge you for the transcript.
Just trust your gut. And your napkin.