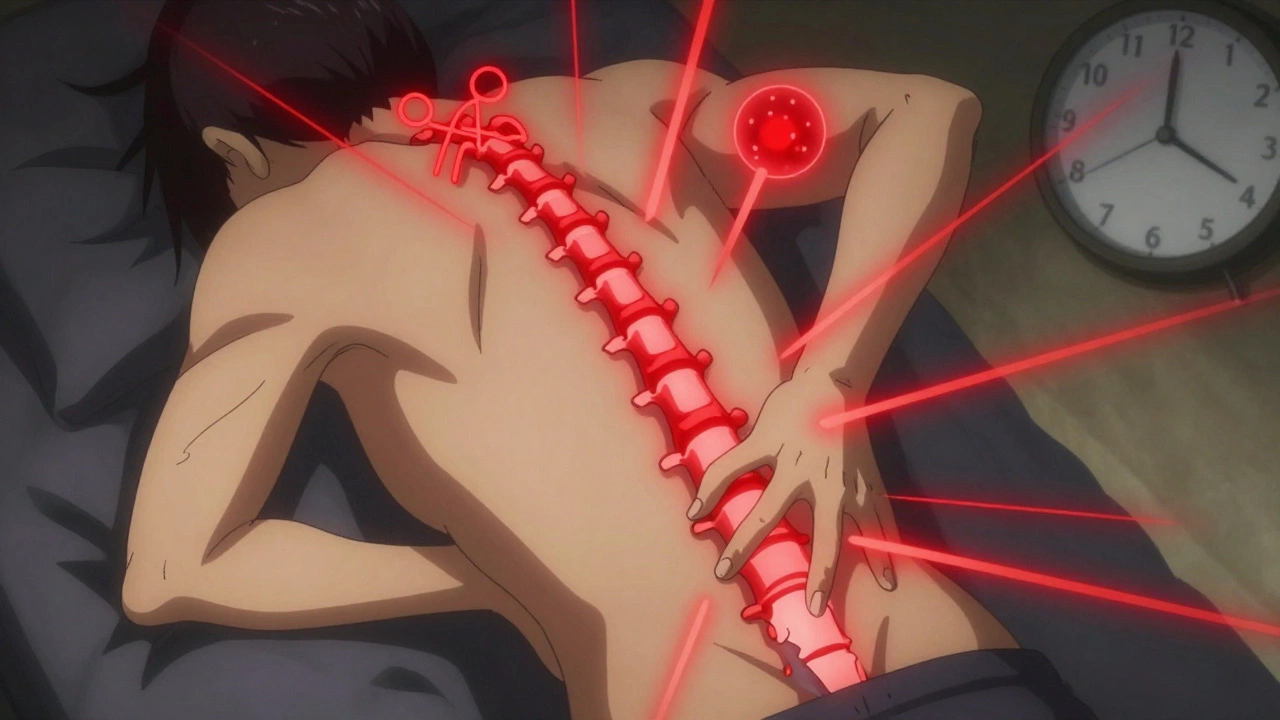
Most people experience back pain at some point. It’s common, often goes away on its own, and doesn’t need scans or surgery. But back pain red flags are the warning signs that tell you something more serious might be going on - and waiting could cost you mobility, nerve function, or even your life.
What Are Back Pain Red Flags?
Red flags aren’t just intense pain. They’re specific clues in your history, symptoms, or physical exam that point to dangerous conditions like spinal infections, tumors, fractures, or nerve damage. These aren’t guesses. They’re based on decades of clinical research and updated guidelines from the American College of Physicians, the American College of Emergency Physicians, and the American College of Radiology.Here’s the reality: 90% of back pain cases are harmless - muscle strains, minor disc issues, or joint irritation. But the other 10%? Those are the ones that need immediate action. Missing them isn’t just a medical error - it’s a legal risk. Malpractice claims tied to missed spinal emergencies make up 1.7% of all emergency medicine lawsuits, according to ACEP data from 2020.
Must-Not-Miss Red Flags
There are five conditions you absolutely cannot overlook. If any of these apply, don’t wait. Don’t take more ibuprofen. Don’t try yoga. Get evaluated now.- Cauda equina syndrome: This is a neurological emergency. Look for loss of bowel or bladder control, numbness in the saddle area (between your legs), or sudden weakness in both legs. MRI is the gold standard - delay beyond 48 hours can lead to permanent paralysis.
- Spinal infection (osteomyelitis or abscess): Fever, unexplained weight loss, night sweats, and pain that doesn’t improve with rest or painkillers are huge red flags. In one study, 78% of patients with spinal infections had pain that didn’t respond to analgesics, compared to just 22% with mechanical back pain.
- Spinal fracture: If you’re over 50, have osteoporosis, or recently fell or been in an accident, any new back pain needs imaging. CT scans detect fractures with 98% accuracy; plain X-rays miss nearly 40% in older adults.
- History of cancer: If you’ve had breast, lung, prostate, or kidney cancer in the past, new back pain could mean the cancer has spread to your spine. The positive likelihood ratio for malignancy jumps to 6.4-15.3 if you have a prior cancer diagnosis.
- Unexplained weight loss or night pain: Pain that wakes you up at night, especially if you’ve lost weight without trying, raises suspicion for tumor or infection. It’s not just discomfort - it’s a signal your body is fighting something serious.
Age Matters - But Not How You Think
You might assume back pain in older people is just “wear and tear.” It’s not always. People over 50, especially over 70, are at much higher risk for vertebral compression fractures. One study found 36.5% of patients over 70 with back pain had fractures - compared to just 9.1% under 50.But younger people aren’t safe either. Back pain in children or teens under 18 is rare and almost always means something more than a pulled muscle. Spinal tumors, infections, or inflammatory conditions like spondylitis are more common in this group than in older adults.
Age isn’t just a number - it’s a risk multiplier. If you’re over 50 and have osteoporosis, steroid use, or a history of trauma, your risk of fracture triples. That’s why guidelines now recommend CT over X-ray for this group - plain films miss too many fractures.
When Imaging Is (and Isn’t) Needed
You don’t need an MRI just because your back hurts. In fact, up to 34% of initial imaging for back pain is inappropriate, according to a review of 1.2 million patients. Unnecessary scans lead to false positives, anxiety, and even unnecessary surgeries.Here’s what the evidence says:
- No red flags? Wait 4-6 weeks. The American Academy of Family Physicians and the American College of Physicians both recommend conservative care - activity, physical therapy, pain relief - before imaging. Most pain improves on its own.
- Red flags? Get imaging now. MRI is the best tool for infections, tumors, and nerve compression. It’s 95% sensitive for cauda equina syndrome. CT is better for fractures - 98% accurate versus X-ray’s 64%.
- Plain X-rays? Limited use. Only use them for older patients with osteoporosis or trauma. They’re not good enough to rule out serious issues.
And here’s the kicker: 65.6% of patients with serious spinal pathology didn’t get the imaging they needed. That’s not just bad luck - it’s systemic under-recognition of red flags.
What If Pain Doesn’t Improve?
Pain that lasts longer than a month is a red flag in itself. A 2018 Spine study found patients who didn’t improve after four weeks were 19.3 times more likely to need surgery than those who got better quickly.This isn’t about being impatient. It’s about recognizing when conservative care isn’t working. If you’ve tried rest, physical therapy, and over-the-counter meds for four weeks and you’re still in pain - especially if it’s radiating down your leg or getting worse - it’s time to see a specialist.
That doesn’t mean you need surgery. But it does mean you need a deeper look - possibly an MRI or referral to a spine specialist or pain management doctor.
What Happens After a Red Flag Is Found?
If you’re flagged for a serious condition, here’s what usually happens next:- Cauda equina: Emergency MRI. If confirmed, surgery within 48 hours is critical to prevent permanent bladder, bowel, or leg damage.
- Spinal infection: Blood tests (CRP, ESR), MRI, and possibly a biopsy. Antibiotics or drainage may be needed. Diagnosis often takes over 18 days - early recognition saves time and tissue.
- Fracture: CT scan. If unstable, you may need bracing or surgery. If stable, conservative care with activity modification.
- Suspected tumor: MRI, biopsy, oncology referral. Early detection improves survival rates dramatically.
Physical therapists and primary care providers are trained to spot these signs. If your provider says, “Let’s wait and see,” but you have any of the red flags above - push back. Ask for imaging. Ask for a referral.
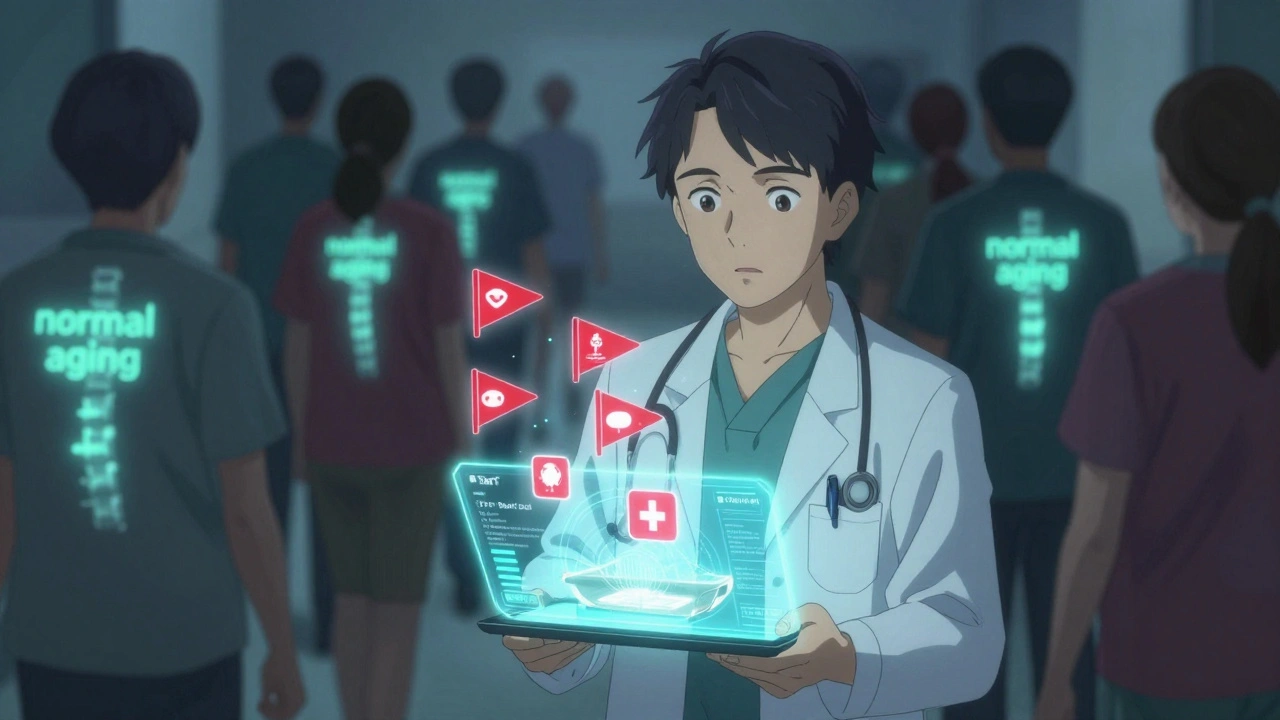
What About New Tech? AI and Ultrasound
The field is evolving. The American College of Radiology’s 2023 update now includes machine learning tools that predict red flags with 89% accuracy - better than traditional screening (76%).Point-of-care ultrasound (POCUS) is also emerging. A 2022 study showed POCUS can detect bladder distension - a sign of nerve compression - with 92% accuracy. This could cut unnecessary MRIs by 35% in emergency rooms.
And in 2024, the American Pain Society is testing a new risk-stratification tool called STarT Back. It uses a short questionnaire to predict who’s at risk for serious pathology - not just pain. Early results show 83% sensitivity, meaning it catches most cases without over-testing.
The Cost of Waiting - and the Cost of Overtesting
Overuse of imaging for back pain costs the U.S. an estimated $3 billion a year. But under-testing? That costs lives.Insurance companies are catching on. Anthem’s policy explicitly denies coverage for imaging without red flags - and has rejected 42% of appeals for unnecessary scans in 2022.
Meanwhile, patients who get unnecessary MRIs are more likely to be told they have “degenerative disc disease” - even if they have no pain. One study found 79% of asymptomatic 80-year-olds showed disc degeneration on MRI. That’s not a diagnosis - it’s normal aging. But it leads to unnecessary fear, more tests, and sometimes, surgery that doesn’t help.
Bottom Line: Know the Signs, Act Fast
Back pain is common. Serious causes are rare - but they’re deadly if missed.If you have any of these, don’t wait:
- Loss of bladder or bowel control
- Unexplained fever or weight loss
- Pain that wakes you up at night
- Pain after trauma, especially if you’re over 50 or on steroids
- History of cancer with new back pain
- Pain that hasn’t improved after 4 weeks
For everyone else - rest, move gently, take OTC pain relief, and give it time. Most cases resolve without scans, shots, or surgery.
Knowing the difference isn’t just smart - it’s life-saving.
Can back pain be serious even if it’s not severe?
Yes. Some of the most dangerous conditions - like spinal infections or early tumors - cause dull, aching pain that doesn’t feel “bad enough” to warrant concern. The key isn’t pain intensity, but whether it’s accompanied by red flags like fever, weight loss, night pain, or neurological symptoms. A mild ache that doesn’t improve after four weeks can be more concerning than a sharp pain that goes away in two days.
Do I need an MRI for every episode of back pain?
No. MRI is only recommended when red flags are present or if pain persists beyond 4-6 weeks despite conservative care. For most people, imaging doesn’t improve outcomes and can lead to unnecessary procedures. Up to 79% of asymptomatic adults over 80 show disc degeneration on MRI - that’s normal aging, not a problem needing treatment.
What if my doctor says my back pain is just “degenerative”?
Degenerative changes are common and often unrelated to pain. If your symptoms match typical mechanical back pain - worse with movement, better with rest, no neurological symptoms - then yes, it’s likely degenerative. But if you have red flags like numbness, weakness, or bowel/bladder changes, ask for further testing. Don’t accept “it’s just aging” if your symptoms are worsening or unusual.
Can physical therapy help if I have red flags?
Physical therapy is helpful for most back pain - but not when red flags are present. If you have signs of infection, fracture, or nerve compression, PT could make things worse. The first step is medical evaluation and imaging. Once serious conditions are ruled out or treated, physical therapy becomes a key part of recovery.
Is it safe to wait a few days if I have mild red flags?
No. If you have cauda equina syndrome, spinal infection, or a recent trauma with possible fracture, waiting even 24-48 hours can lead to permanent damage. These are emergencies. Go to the ER or call your doctor immediately. Don’t wait to see if it gets worse - by then, it may be too late.
Are blood tests useful for diagnosing back pain causes?
Yes, for certain conditions. If infection or inflammation is suspected, blood tests like CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate) can help. Levels above 30 mg/L and 50 mm/hr, respectively, strongly suggest spinal infection. These aren’t used alone, but they’re valuable tools when combined with symptoms and imaging.
Next Steps If You’re Concerned
If you’re unsure whether your back pain needs attention, start here:- Check for red flags - especially neurological symptoms, fever, or unexplained weight loss.
- If any red flags are present, go to urgent care or the ER immediately.
- If no red flags but pain lasts more than 4 weeks, schedule a visit with your primary doctor or a spine specialist.
- Keep a pain journal: note when it hurts, what makes it better/worse, and any new symptoms.
- Don’t pressure your provider for imaging unless red flags are present - unnecessary scans do more harm than good.
Back pain doesn’t always mean something’s wrong. But when it does - knowing the signs can change everything.

11 Comments
Taylor Dressler
10 December, 2025Really well-structured breakdown. I’ve seen too many patients delay care because they thought, 'It’s just back pain.' The cauda equina warning alone is worth printing and taping to your fridge. If you lose control of your bladder or feel numb between your legs, don’t call your buddy for advice-call 911. No exceptions.
Also, love the emphasis on imaging overuse. I’m a PT, and I see patients come in terrified because their MRI showed 'degenerative disc disease'-but they’ve never had trauma or red flags. It’s not pathology, it’s aging. We need better public education on that.
And yes, POCUS for bladder distension? That’s a game-changer for ERs. Saves time, money, and avoids unnecessary MRIs. Kudos for including emerging tech.
One thing I’d add: don’t ignore progressive weakness. Even without numbness or bowel issues, if your foot starts dropping or you can’t climb stairs like you used to, that’s a red flag too. Nerve compression doesn’t always scream-it whispers, and we miss it.
Thanks for this. I’m sharing it with my students tomorrow.
Aidan Stacey
11 December, 2025OH MY GOD. I almost ignored my own back pain last year. Thought it was 'just a pulled muscle' after moving furniture. Then I started waking up at 3 a.m. sweating like I was in a sauna, and I lost 12 pounds without trying. My doctor said 'maybe stress.'
I went to the ER anyway. Turned out to be spinal abscess. Spent 3 weeks in the hospital. Had two surgeries. Still rehabbing.
THIS POST SAVED MY LIFE. I’m telling everyone I know. If you have night pain + weight loss + fever? GO. NOW. Don’t wait for a 'better day.' There won’t be one.
Jean Claude de La Ronde
12 December, 2025So let me get this straight-we’re supposed to panic every time someone says 'back pain' and then immediately book an MRI? Wow. I didn’t know we’d entered the era of medical paranoia.
I mean, sure, some people have tumors. But so do some people have aliens in their kidneys. Should we all get whole-body scans just in case?
Also, 'degenerative disc disease' is basically just a fancy way of saying 'you’re alive.' You’re not broken. You’re just… older. Like a toaster with a frayed cord. Doesn’t mean it’s gonna explode.
And why is every article now about 'red flags'? It’s like medical advice has become a horror movie trailer. 'You think your back hurts? WAIT TIL YOU HEAR WHAT HAPPENS NEXT.'
Also, 'STarT Back'? Sounds like a bad yoga studio. I’m skeptical.
Anyway. I’m gonna go stretch. And maybe buy a toaster.
Courtney Blake
13 December, 2025Of course the system fails. Why? Because doctors are overworked, underpaid, and trained to treat symptoms, not people. And insurance? They don’t care if you’re paralyzed-they care if you filed the right code.
And don’t even get me started on how they call it 'degenerative' like it’s some natural law. It’s not. It’s the result of decades of sitting, poor posture, and corporate America telling us to 'just push through.'
Meanwhile, the real culprits-sedentary jobs, opioid prescriptions, and lack of physical therapy access-are ignored. We’re treating the symptom, not the cause. And then we blame the patient for not 'healing faster.'
Also, 65% of serious cases go undiagnosed? That’s not negligence. That’s a systemic massacre. 😔
Doris Lee
13 December, 2025Thank you for this. I’ve been dealing with back pain for months and kept thinking I was being dramatic. But when I started waking up at night and couldn’t sit for more than 10 minutes without shifting, I finally went in.
Turns out, nothing serious-just a pinched nerve from sitting wrong at my desk. But I wouldn’t have known if I hadn’t read this.
So if you’re unsure? Go get checked. You deserve to move without pain. And you’re not overreacting if you’re worried.
Take care of yourself, friends. You’re worth it. ❤️
Frank Nouwens
14 December, 2025While the clinical guidelines presented are generally sound and evidence-based, one must acknowledge the socioeconomic disparities that influence access to timely imaging and specialist referral. In many rural and underserved communities, the absence of MRI facilities or neurology consults renders even the most accurate red-flag identification clinically inert.
Furthermore, the implicit assumption that patients possess the health literacy to self-identify red flags is not universally valid. Language barriers, educational disparities, and cultural norms around medical authority may prevent timely escalation.
Thus, while individual vigilance is commendable, systemic reform-including community health worker programs and mobile imaging units-is equally critical to reducing morbidity.
Thank you for a rigorously referenced and thoughtful contribution.
Kaitlynn nail
14 December, 2025So… if you’re over 50 and feel a twinge? MRI. If you’re 25 and your back hurts after lifting a bag? Chill.
Also, 'degenerative disc disease' is just a fancy way of saying 'you’re old.'
And yes, I’m saying this while sitting on my couch in sweatpants.
Also, AI? Cool. But can it tell if my cat stepped on my back? Probably not.
Anyway. I’m gonna go drink water and ignore my spine.
Aileen Ferris
15 December, 2025Wait, so if you have back pain and you’re over 50, you need a CT? But if you’re under 50 and have the same pain, you’re fine? That’s not science, that’s ageism.
And who decided 'night pain' is a red flag? Maybe I just sleep weird. Maybe I had a bad dream. Maybe I’m stressed.
Also, 'unexplained weight loss'? I lost 5 pounds because I stopped eating carbs. Is that cancer? Or just keto?
I’m not saying this isn’t important, but the fear-mongering is getting out of hand. We used to just take ibuprofen and call it a day.
Also, I’m Irish. We don’t do 'red flags.' We do 'it’ll pass.'
Michelle Edwards
16 December, 2025I’ve been there. Pain for 6 weeks. Thought I was being weak. Then I started getting tingles down my leg. I didn’t panic-I just called my doctor and said, 'I’m not getting better.'
They sent me for an MRI. Turns out, a small herniation. No surgery. Just PT and stretches.
But if I’d waited another month? It could’ve been worse.
You don’t have to be dramatic. You just have to be consistent. Track your pain. Listen to your body. And don’t let anyone tell you it’s 'just stress.'
You’ve got this. 💪
Sarah Clifford
18 December, 2025MY BACK HURTS AND I’M 32 AND I’VE NEVER HAD A FALL AND NOW I’M SCARED I HAVE SPINAL CANCER
JK I’M JUST SITTING TOO LONG
BUT LIKE. WHAT IF?
WHY IS EVERYTHING A RED FLAG NOW?
WHEN DID BACK PAIN BECOME A THRILLER MOVIE?
IM JUST TRYING TO GET TO THE FRIDGE
Ben Greening
19 December, 2025The data presented is methodologically sound and aligns with current clinical guidelines from the ACP and ACEP. However, the emphasis on red flags may inadvertently contribute to physician anxiety and defensive medicine, particularly in high-volume primary care settings where time constraints limit comprehensive history-taking.
It is also worth noting that the sensitivity of patient-reported symptoms for conditions such as spinal infection remains suboptimal; many patients with osteomyelitis present with minimal or atypical symptoms.
Future iterations of risk-stratification tools should integrate longitudinal symptom tracking and biomarker trends rather than relying on static clinical flags.
Well-researched and clinically relevant.