Bleeding Risk Calculator for Dual Antiplatelet Therapy
Bleeding Risk Assessment
This tool calculates your bleeding risk score based on the PRECISE-DAPT criteria. A score of 25 or higher indicates high bleeding risk.
Your Bleeding Risk Score
What This Means for Your Dual Antiplatelet Therapy
Key factors in your score:
When you’ve had a heart stent placed or survived a heart attack, doctors often prescribe dual antiplatelet therapy-a combo of aspirin and another drug like clopidogrel, prasugrel, or ticagrelor. It’s meant to keep your blood from clotting inside the stent, which could trigger another heart attack or even death. But here’s the catch: the same drugs that save your life can also make you bleed more easily. A minor cut, a nosebleed, or even a stomach ulcer can turn into a serious problem. Managing these bleeding risks isn’t optional-it’s part of surviving and staying well after a cardiac event.
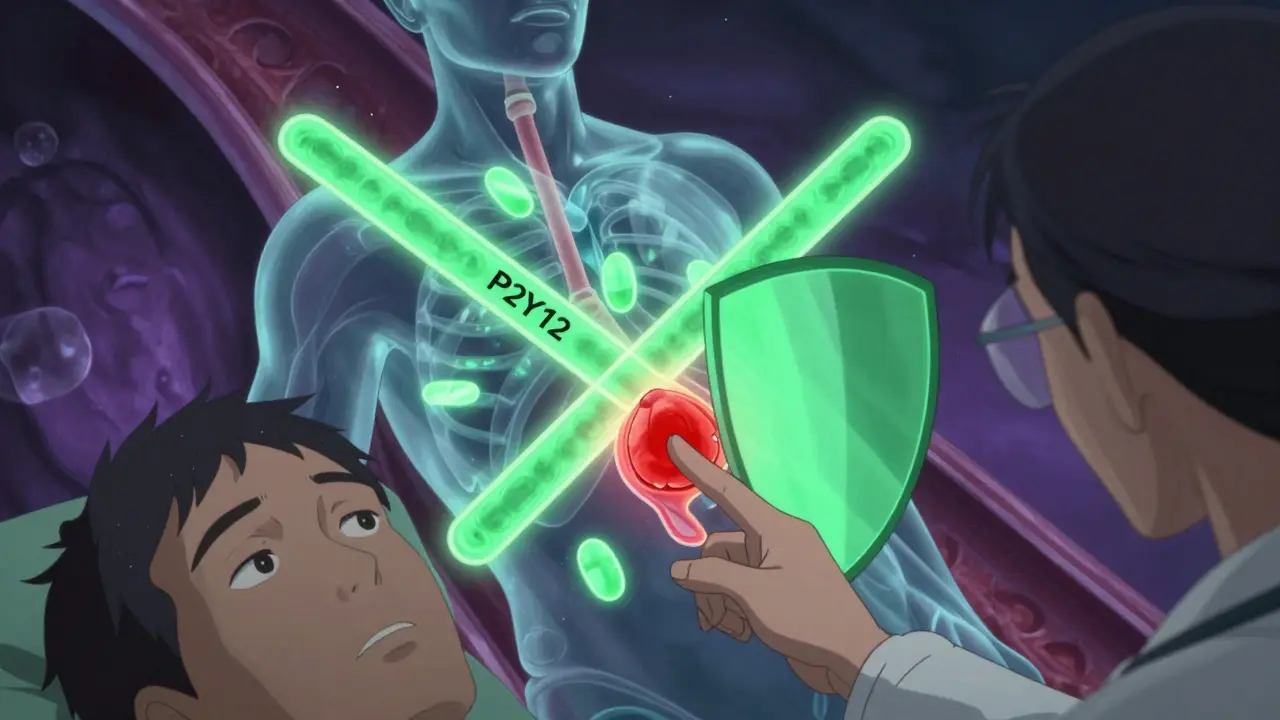
What Dual Antiplatelet Therapy Really Does
Dual antiplatelet therapy, or DAPT, works by blocking platelets-the tiny blood cells that clump together to form clots. Aspirin stops one pathway; the P2Y12 inhibitor (like clopidogrel or ticagrelor) blocks another. Together, they’re stronger than either drug alone. This combo became standard after the CURE trial in 2001 showed it cut heart attacks and strokes by about 20% in high-risk patients. Since then, it’s been the go-to treatment after stent placement or heart attack.
But every benefit has a cost. The PLATO trial found that while DAPT reduces major heart events by 15-30%, it increases the risk of major bleeding by 1-2% compared to using just one antiplatelet drug. That might sound small, but in real life, that means one extra person out of every 50 on DAPT will have a bleeding event serious enough to require hospitalization or a blood transfusion.
Which Drugs Are Used-and How They Differ
Not all DAPT regimens are the same. The three main P2Y12 inhibitors used with aspirin are:
- Clopidogrel (75 mg daily): Older, cheaper, and less powerful. Bleeding risk is lower, but so is protection against clots.
- Prasugrel (10 mg daily, 5 mg if over 75 or under 60 kg): Faster, stronger, and better at preventing heart events-but it also bleeds more. Not recommended for older adults or those with low body weight.
- Ticagrelor (90 mg twice daily): Most potent. Reduces heart attacks and death more than clopidogrel, but increases major bleeding by 27% according to the TRITON-TIMI 38 trial. Also causes shortness of breath in about 15% of users.
The 2023 European Society of Cardiology guidelines now recommend ticagrelor or prasugrel for most patients unless they’re at high bleeding risk. For those patients, clopidogrel is often the safer choice.
Who’s at Highest Risk for Bleeding?
Not everyone on DAPT will bleed. But some people are much more likely to. Doctors use the PRECISE-DAPT score to figure this out. A score of 25 or higher means you’re at high bleeding risk. Factors that push your score up include:
- Age 75 or older
- History of bleeding (even a nosebleed that needed packing)
- Low hemoglobin (anemia)
- Low kidney function (creatinine clearance under 60)
- Low platelet count
- Taking blood thinners like warfarin or apixaban
A 2021 consensus defined high bleeding risk as a 4% or higher chance of severe bleeding within a year. That’s not rare-it’s common. About 45% of PCI patients in Europe now meet this criteria, up from just 15% in 2017.
The Bleeding You Don’t See (But Feel)
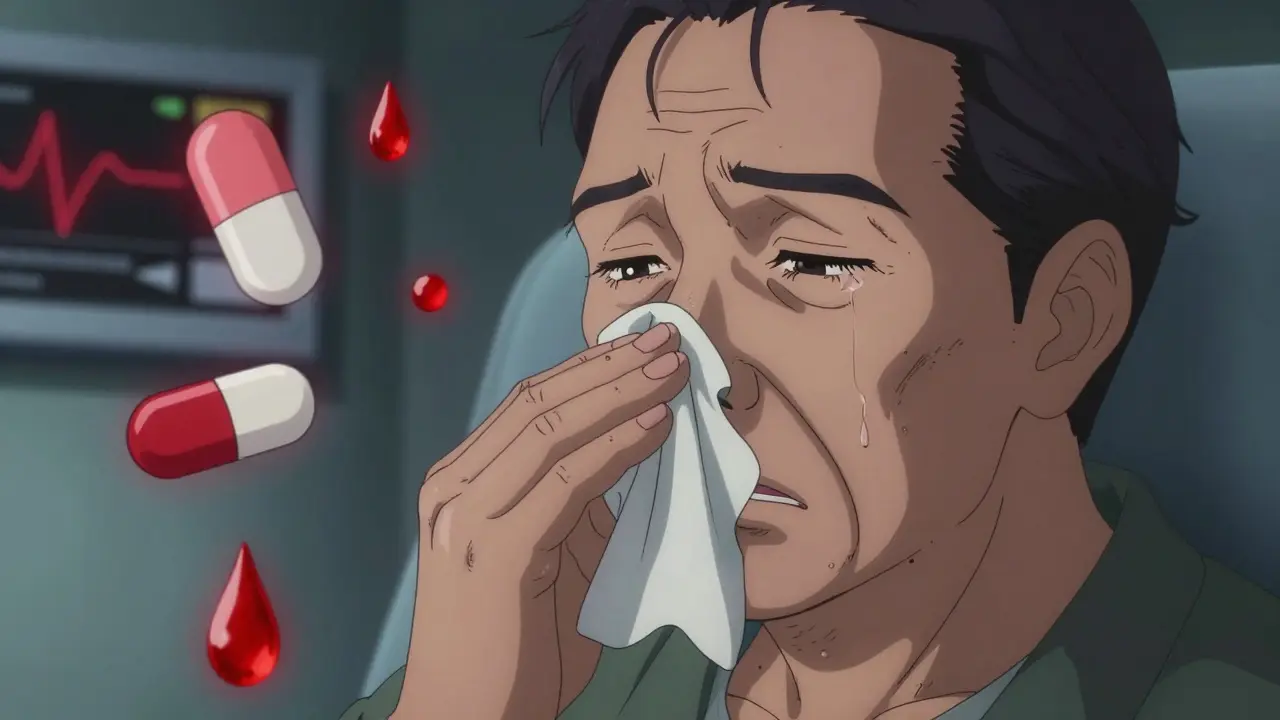
Most people worry about life-threatening bleeding-like a brain bleed or stomach ulcer. But the real problem for many is the “nuisance bleeding” that doesn’t land you in the ER but ruins your daily life.
The TALOS-AMI trial tracked 2,583 heart attack patients on ticagrelor. In the first month, 15.2% had minor bleeding: nosebleeds, bruising, bleeding gums, or blood in stool. These weren’t emergencies, but they scared patients. One in three stopped taking their medication because of it. Nearly 19% quit entirely within six months. That’s dangerous-stopping DAPT too early doubles or triples your risk of stent clotting.
Patients on Reddit and in surveys reported:
- 83% had gastrointestinal bleeding (black stools, stomach pain)
- 32% had frequent nosebleeds needing nasal packing
- 15% said even a small cut bled for over 20 minutes
And the emotional toll? 68% said they were anxious about daily activities. 41% skipped social events because they feared bleeding in public. That’s not just a medical issue-it’s a quality-of-life crisis.
How to Reduce Bleeding Without Losing Protection
The good news? You don’t have to choose between bleeding and clots. There are smarter ways to manage DAPT.
1. Shorten the duration
For years, everyone got 12 months of DAPT. Now, we know that’s too long for many. The MASTER DAPT trial (2022) showed that in high-risk patients, stopping DAPT after just one month and switching to aspirin alone cut major bleeding by 6.9% over two years-with no increase in heart attacks or death.
The Onyx ONE trial (2020) confirmed this: 1-month DAPT followed by aspirin alone was safer than 12 months, without raising the risk of clots.
2. De-escalate the drug
If you’re on ticagrelor or prasugrel and you’re bleeding, switching to clopidogrel after 1-3 months can cut bleeding by 25-30% without losing protection. The TALOS-AMI trial showed a 2.1% drop in major bleeding events with this switch. And patients reported feeling better-72% saw improved quality of life scores.
3. Don’t stop cold turkey
Stopping DAPT before 6 months (if you’re not high-risk) increases stent clotting risk by 2-3 times. The PARIS registry found that patients who quit early were far more likely to die or have another heart attack. Never stop on your own. Talk to your doctor.
What to Do If You Start Bleeding
If you notice:
- Bloody or black stools
- Vomiting blood or coffee-ground material
- Unexplained bruising or swelling
- Nosebleeds lasting more than 15 minutes
- Headache with dizziness (possible brain bleed)
Call your doctor or go to the ER. Don’t wait.
For minor bleeding, like a nosebleed or small cut:
- Apply direct pressure for at least 10 minutes
- Don’t take NSAIDs like ibuprofen or naproxen-they make bleeding worse
- Use acetaminophen (paracetamol) for pain instead
For major bleeding, hospitals follow strict protocols. Platelet transfusions are only recommended for life-threatening bleeding in patients who took clopidogrel within the last 5 days. One unit can restore about 30% of platelet function in two hours. But there’s no antidote for ticagrelor or prasugrel yet-unlike warfarin, which has vitamin K, or dabigatran, which has idarucizumab. That’s a big gap in care.
What You Can Do Right Now
You’re not powerless. Here’s your action plan:
- Ask your doctor for your PRECISE-DAPT score. If it’s 25 or higher, ask if you qualify for shortened or de-escalated DAPT.
- Keep a bleeding journal: note when, where, and how long bleeding lasts. Bring it to appointments.
- Never stop DAPT without talking to your cardiologist-even if you feel fine.
- Use acetaminophen, not ibuprofen or aspirin (unless it’s your prescribed dose).
- Tell every doctor you see-including dentists-that you’re on DAPT. Some procedures (like tooth extractions) may need adjustments.
- Ask if you can switch from ticagrelor to clopidogrel after 1-3 months. It’s safer and just as effective for many.
The Future: Personalized DAPT Is Coming
The days of one-size-fits-all DAPT are ending. The DAPT-PLUS registry, launched in 2023 with $4.2 million in NIH funding, is using AI to predict who will bleed and who won’t. By 2028, experts predict 90% of stent patients will get personalized DAPT plans-shorter for those at high bleeding risk, longer for those at high clot risk.
Researchers are even testing reversal agents for ticagrelor. Two candidates are already in early trials. If they work, they could be game-changers.
For now, the best tool you have is information. Know your risk. Ask questions. Don’t accept bleeding as normal. And never assume that more drugs = better protection. Sometimes, less is more.
Can I stop dual antiplatelet therapy if I’m bleeding?
Never stop DAPT on your own. Stopping too early-especially before 6 months-can cause stent clots, which often lead to heart attacks or death. If you’re bleeding, contact your doctor immediately. They may adjust your dose, switch you to a safer drug like clopidogrel, or shorten the treatment time-but only under medical supervision.
Is clopidogrel safer than ticagrelor for bleeding?
Yes, clopidogrel carries a lower risk of major bleeding than ticagrelor-about 27% lower based on the TRITON-TIMI 38 trial. However, it’s also less effective at preventing heart attacks and strokes. For high-bleeding-risk patients, switching from ticagrelor to clopidogrel after 1-3 months reduces bleeding without increasing heart events. This is now a recommended strategy in recent guidelines.
How long should I stay on dual antiplatelet therapy?
For standard-risk patients, 6-12 months is typical after a drug-eluting stent. For high-bleeding-risk patients, 1-3 months of DAPT followed by aspirin alone is now supported by strong evidence. Your doctor should use your PRECISE-DAPT score to decide. Don’t assume 12 months is right for you-personalized plans are the new standard.
Can I take ibuprofen or aspirin for headaches while on DAPT?
Avoid ibuprofen, naproxen, or other NSAIDs-they increase bleeding risk and can interfere with aspirin’s effect. For headaches, use acetaminophen (paracetamol) instead. If you’re already on low-dose aspirin (75-100 mg) as part of DAPT, don’t take extra aspirin unless your doctor tells you to. More isn’t better-it’s riskier.
Do I need regular blood tests to check if DAPT is working?
No. The French Working Group and major cardiology societies agree there’s no proven benefit to routine platelet function testing. These tests are expensive, inconsistent, and don’t change outcomes. Doctors should rely on your clinical history, bleeding signs, and risk scores-not lab results-to manage your therapy.
What if I need dental work or surgery?
You usually don’t need to stop DAPT for minor procedures like fillings, root canals, or tooth extractions. The European Association of Percutaneous Cardiovascular Interventions says DAPT is safe for these. For major surgery, your cardiologist and surgeon will decide together. In most cases, continuing DAPT is safer than stopping it. Never stop without their approval.

10 Comments
Alexandra Enns
23 January, 2026Let me tell you something the medical industrial complex doesn't want you to know - DAPT is a scam. They push these drugs because they make billions, not because they're safe. I've seen patients turn into walking bruises. One guy bled out from a paper cut. And now they want us to take it for 12 months? Are you kidding me? The real solution is lifestyle - stop eating processed crap, start walking, and ditch the pills. Pharma doesn't profit from kale.
Marie-Pier D.
24 January, 2026Hi everyone, I just wanted to say thank you for sharing this - it’s so hard to find clear info on this stuff. My mom was on ticagrelor and had 3 nosebleeds in one week. She was terrified to even brush her teeth. We switched her to clopidogrel after 6 weeks and her quality of life improved overnight 😊 She still takes aspirin, and she’s been stable for 8 months now. You’re not alone. Talk to your doc. You’ve got this 💪
Heather McCubbin
26 January, 2026So let me get this straight - we’re supposed to believe that bleeding gums and black stools are just 'nuisance' side effects? This is what happens when doctors treat patients like lab rats. They don’t care if you're scared to leave the house. They care about their stats. And now they want to shorten DAPT? That’s just the next phase of cost-cutting disguised as innovation. Wake up people. This system is rigged.
Tiffany Wagner
27 January, 2026I’ve been on DAPT for 18 months after my stent and honestly I didn’t realize how much anxiety I had until I switched to clopidogrel. No more panic every time I sneeze. My doctor said 3 months was enough for me since I’m low risk. I didn’t know I could ask for that. Just wanted to say - ask. You deserve to feel safe.
venkatesh karumanchi
27 January, 2026From India, I can confirm - clopidogrel is the only option for most of us. Ticagrelor costs 5x more and we don’t have the luxury of expensive drugs. But guess what? Our outcomes are just as good. The real issue is access, not the drug. If your doctor pushes the expensive one without checking your finances, find a new one. Your life isn’t a profit margin.
lorraine england
28 January, 2026So many people don’t realize that stopping DAPT early isn’t the problem - it’s stopping without a plan. My cousin quit cold turkey because he was scared of bleeding. Ended up with a clot in his stent. Died two weeks later. Please don’t be that person. Talk to your cardiologist. Keep a journal. Ask about PRECISE-DAPT. You’re not being paranoid - you’re being smart.
Kevin Waters
29 January, 2026Just had a 3-month follow-up with my cardiologist and we switched me from ticagrelor to clopidogrel. Bleeding stopped immediately. No more black stools, no more scary bruising. I was worried it wouldn’t be as effective - but my repeat angiogram showed perfect stent patency. This isn’t cutting corners. This is precision medicine. Trust the data, not the fear.
Kat Peterson
30 January, 2026Okay but have you heard about the DAPT-PLUS registry? 😳 It’s funded by the NIH and they’re using AI to predict who bleeds. That means your DNA is being scanned, your habits are being tracked, and your insurance company is gonna use this to deny coverage if you're 'high risk'. This isn’t healthcare - it’s predictive profiling. I’m not taking this drug until I know who’s watching me.
Helen Leite
30 January, 2026They’re lying about the bleeding stats. I saw a video on YouTube where a nurse said the trials hide the real numbers. They count nosebleeds as 'minor' but if you bleed for 20 minutes, that’s not minor. That’s trauma. And why is there no antidote for ticagrelor? Because if there was, they’d lose control. Big Pharma owns the FDA. I’m not taking it. Period.
blackbelt security
1 February, 2026My dad’s on clopidogrel after a stent. He’s 78. Bleeding? Zero. Heart issues? None. He walks 2 miles every morning. Eats veggies. Sleeps 7 hours. No drama. No panic. Just discipline. You don’t need fancy drugs. You need consistency. Start there.