High blood pressure doesn’t come with warning signs. You might feel fine, but your arteries are under constant strain. Left unchecked, it can lead to heart attack, stroke, or kidney failure. That’s why millions of people take blood pressure medication every day - not because they’re sick, but because they’re trying to stay that way. The problem? Many people stop taking their meds because of side effects, confusion, or the false belief that if they feel okay, the medicine isn’t working. The truth is, blood pressure meds are one of the most important tools you have to protect your long-term health - if you use them right.
How Blood Pressure Medications Work
Your blood pressure is the force of blood pushing against your artery walls. When it’s too high, your heart and blood vessels work harder than they should. Blood pressure medications don’t cure hypertension. They manage it by targeting different parts of your body’s control system.There are ten main classes of these drugs, each with a different job:
- Diuretics (like hydrochlorothiazide) help your kidneys flush out extra salt and water. Less fluid in your bloodstream means lower pressure.
- Beta-blockers (like metoprolol) slow your heart rate and reduce how hard your heart pumps. They’re especially useful if you’ve had a heart attack.
- ACE inhibitors (like lisinopril) block a chemical that narrows blood vessels. This lets your arteries relax.
- ARBs (like losartan) do something similar but block the same chemical at a different point - often without the dry cough that ACE inhibitors cause.
- Calcium channel blockers (like amlodipine) prevent calcium from entering heart and artery cells, which relaxes your blood vessels.
- Alpha-blockers (like doxazosin) stop nerves from tightening blood vessels.
- Alpha-beta blockers (like carvedilol) combine the effects of alpha and beta-blockers.
- Central agonists (like clonidine) send signals to your brain to reduce nerve impulses that raise blood pressure.
- Vasodilators (like hydralazine) directly relax the muscles in your artery walls.
- Renin inhibitors (like aliskiren) block an enzyme your kidneys release to start the chain reaction that raises blood pressure.
Most people start with one of four: thiazide diuretics, calcium channel blockers, ACE inhibitors, or ARBs. Which one? It depends on your age, race, other health conditions, and how your body responds.
Common Side Effects - And What to Do About Them
Side effects are why so many people quit taking their meds. But not all side effects are the same, and most can be managed.Here’s what you might experience with each class:
- Diuretics: You’ll need to pee more - especially at first. Some people get low potassium, dizziness, or gout flare-ups. Eating bananas or taking a potassium supplement (if your doctor says it’s safe) can help.
- Beta-blockers: Fatigue, cold hands and feet, trouble sleeping, and reduced sex drive are common. If you’re diabetic, they can hide signs of low blood sugar. Talk to your doctor if these hit hard.
- ACE inhibitors: A persistent dry cough affects 10-20% of users. It’s not dangerous, but it’s annoying. If it sticks around, switching to an ARB usually fixes it. Rarely, they can cause swelling of the face or throat (angioedema) - that’s an emergency.
- ARBs: Fewer side effects than ACE inhibitors, but still carry risk of high potassium and, like ACE inhibitors, are unsafe during pregnancy.
- Calcium channel blockers: Amlodipine can cause swollen ankles, flushing, dizziness, or gum swelling. Good oral hygiene helps with the gum issue. Verapamil might cause constipation.
- Alpha-blockers: Can cause dizziness when standing up quickly (orthostatic hypotension). Take your first dose at bedtime, and stand up slowly.
Some side effects fade after a few weeks as your body adjusts. Others don’t. If you’re struggling, don’t just stop. Call your doctor. There’s almost always another option.
Who Gets Which Medication - And Why
There’s no one-size-fits-all. Your doctor doesn’t just pick a pill at random. They look at your whole picture.For example:
- If you’re Black and have high blood pressure, thiazide diuretics or calcium channel blockers tend to work better than ACE inhibitors or ARBs.
- If you have diabetes or kidney disease, ACE inhibitors or ARBs are preferred because they protect your kidneys.
- If you’ve had a heart attack, beta-blockers are often added to reduce future risk.
- If you’re over 65, doctors often start with lower doses because older bodies react more strongly to meds.
- If you’re pregnant, ACE inhibitors, ARBs, and renin inhibitors are strictly off-limits. Methyldopa or labetalol are safer choices.
For people with stage 2 hypertension (140/90 or higher), guidelines now recommend starting with two medications at once - not one. That’s because most people need more than one drug to get their numbers down. Combining a diuretic with a calcium channel blocker, or an ACE inhibitor with a thiazide, is common and effective.
Safety Risks - What to Avoid
Some combinations can be dangerous.Don’t mix:
- ACE inhibitors + ARBs: This doesn’t give you better control - it just raises your risk of kidney damage and dangerously high potassium levels.
- ACE inhibitors + NSAIDs (like ibuprofen or naproxen): These can cause sudden kidney failure, especially in older adults or those with existing kidney issues.
- Beta-blockers + certain asthma meds: If you have asthma or COPD, some beta-blockers can trigger severe breathing problems. Your doctor will pick one that’s safer.
- Diuretics + potassium supplements: Unless your doctor tells you to, don’t take extra potassium. Too much can cause irregular heartbeat.
Also, don’t skip doses or double up if you forget one. If you miss a dose, take it as soon as you remember - unless it’s almost time for the next one. Then skip the missed one. Never double up to make up for it.

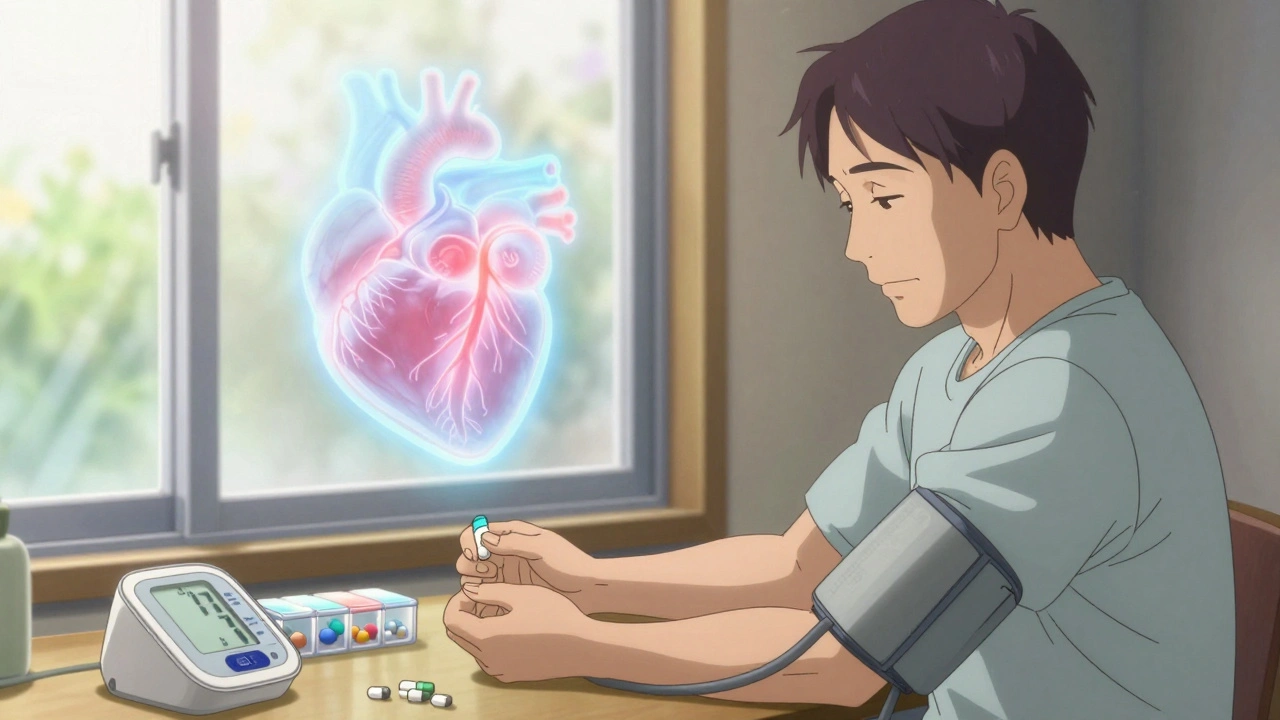
Sticking With Your Meds - The Real Challenge
Here’s the hard truth: about half of people stop taking their blood pressure meds within a year. Why? They feel fine. They hate the side effects. They forget. Or they think it’s not necessary.But high blood pressure is silent. It’s not causing you pain today - but it’s slowly damaging your heart, brain, and kidneys. Stopping your meds is like turning off the alarm on a fire detector. The fire’s still burning.
Here’s how to stay on track:
- Use a pill organizer - especially if you take multiple meds.
- Set phone reminders for when to take your pills.
- Keep your meds in the same spot - next to your toothbrush, coffee maker, or breakfast plate.
- Don’t wait until your next appointment to mention side effects. Call your doctor sooner.
- Ask about combination pills. Some meds come in one tablet (like lisinopril + hydrochlorothiazide), making it easier to remember.
Studies show that people who use apps to track their meds and blood pressure are 15-20% more likely to stay on schedule. It’s not magic - it’s just making it easier to do the right thing.
What’s Next? Personalized Medicine and New Tools
The future of blood pressure treatment is getting smarter. Researchers are studying how your genes affect how you respond to certain drugs. For example, some people metabolize beta-blockers faster than others - meaning they need a higher dose. Others have a genetic trait that makes ACE inhibitors work better for them.While we’re not there yet, doctors are starting to use tools like home blood pressure monitors more regularly. If you’re taking meds, check your pressure at home once or twice a week. Write it down. Bring it to your appointments. It gives your doctor a clearer picture than a single reading in the office.
And for those with hard-to-control blood pressure - even after three or four meds - new drugs are being tested. But for now, the big wins still come from the classics: diuretics, calcium channel blockers, ACE inhibitors, and ARBs - used wisely, safely, and consistently.
Managing high blood pressure isn’t about perfection. It’s about persistence. You don’t need to take your pill at exactly 7:03 a.m. every day. You just need to take it most days. And if you slip up? Start again the next day. Your heart doesn’t need a perfect patient. It just needs you to keep showing up.
Can I stop taking blood pressure medication if my numbers are normal?
No - not without talking to your doctor. Normal blood pressure on medication means the drug is working, not that your condition is cured. Stopping suddenly can cause your pressure to spike, sometimes dangerously. Some people can reduce or stop meds after major lifestyle changes (like losing weight or cutting salt), but only under medical supervision.
Which blood pressure medication has the least side effects?
There’s no single answer - it depends on you. For many, ARBs like losartan have fewer side effects than ACE inhibitors because they don’t cause dry cough. Calcium channel blockers like amlodipine are often well-tolerated, though they can cause swollen ankles. Diuretics are effective but can cause frequent urination and low potassium. The best option is the one that controls your pressure with the fewest issues for your body.
Is it safe to take blood pressure meds with other supplements?
Some supplements can interfere. Licorice root can raise blood pressure. St. John’s Wort can reduce the effect of some meds. Potassium supplements can be dangerous if you’re on ACE inhibitors or ARBs. Always tell your doctor or pharmacist what supplements you’re taking - even if you think they’re "natural" and harmless.
Why do some people need two or three blood pressure pills?
High blood pressure is caused by multiple factors - fluid volume, artery stiffness, heart rate, hormone activity. One pill usually only targets one of these. Combining drugs from different classes hits more targets at once. About 70% of people need two or more medications to reach their goal. It’s not a failure - it’s standard care.
Can blood pressure meds damage your kidneys?
Actually, most protect your kidneys - especially ACE inhibitors and ARBs. But combining them with NSAIDs (like ibuprofen) or taking them when you’re dehydrated can cause sudden kidney injury. That’s why your doctor checks your kidney function and potassium levels regularly. The meds themselves don’t damage kidneys - improper use or drug interactions might.

9 Comments
Ryan Brady
8 December, 2025Ugh, another drug pusher article. 🤮 My BP was fine until I started taking that junk. Now I’m dizzy, tired, and my dick won’t work. Just eat less salt and chill. 🙄
Raja Herbal
10 December, 2025Ah yes, the grand pharmaceutical symphony - where every note is a side effect and the conductor is a 3-minute consult with a doctor who’s already late for his next patient. 🙃
Lola Bchoudi
11 December, 2025Let’s clarify the pharmacodynamics here: ACEi/ARBs are first-line for CKD and DM due to their renoprotective RAAS modulation. Diuretics reduce preload via natriuresis - critical for volume-overloaded HTN. Calcium channel blockers target vascular smooth muscle calcium influx - especially effective in elderly and Black populations per JNC8. Compliance hinges on pill burden reduction - fixed-dose combos improve adherence by 22% per meta-analysis. Don’t just stop. Optimize.
Morgan Tait
12 December, 2025You know what they don’t tell you? The FDA gets paid by Big Pharma to greenlight these pills. 🤫 I’ve been tracking my BP with a $20 wrist monitor - it’s always lower than the clinic. Coincidence? I think not. They want you dependent. They’re injecting nanoparticles to keep you docile. And that dry cough? That’s the government’s way of silencing you. 😷💉 I quit all meds. Now I drink apple cider vinegar, stand on copper mats, and chant at the moon. My BP’s 110/70. Coincidence? I think not.
Darcie Streeter-Oxland
14 December, 2025The assertion that 'blood pressure meds are one of the most important tools' is, in my estimation, a gross oversimplification of a multifactorial physiological condition. One is led to believe that pharmacological intervention is tantamount to moral responsibility, whereas lifestyle modification remains underemphasised in public discourse. The data, however, is not so unequivocal.
Steve Sullivan
15 December, 2025bro i was on lisinopril and it made me cough like a smoker with a cold 😭 then i switched to amlodipine and my ankles swelled like i was pregnant. i just started taking garlic and yoga and my bp is better than my ex’s attitude. who needs pharma when you got vibes? 🙏🌿
Arun Kumar Raut
16 December, 2025I used to think meds were the only way. Then I lost 40 lbs, stopped eating fried food, and walked 30 mins every day. My BP dropped without any pills. Not saying everyone can do this - but don’t give up hope. Small steps matter. You got this.
precious amzy
16 December, 2025The very premise of this article assumes that hypertension is a disease to be medicated rather than a physiological adaptation to systemic dysfunction - a paradigm steeped in reductionist biomedicine and industrial-capitalist hegemony. One wonders whether the true pathology lies not in the arteries, but in the epistemological framework that pathologizes natural variation.
Carina M
16 December, 2025It is patently irresponsible to suggest that 'sticking with your meds' constitutes an act of moral virtue. Such rhetoric infantilizes the patient and obfuscates the profound ethical quandaries surrounding long-term pharmaceutical dependency. One does not become a better human by ingesting synthetic compounds - one becomes a compliant consumer.