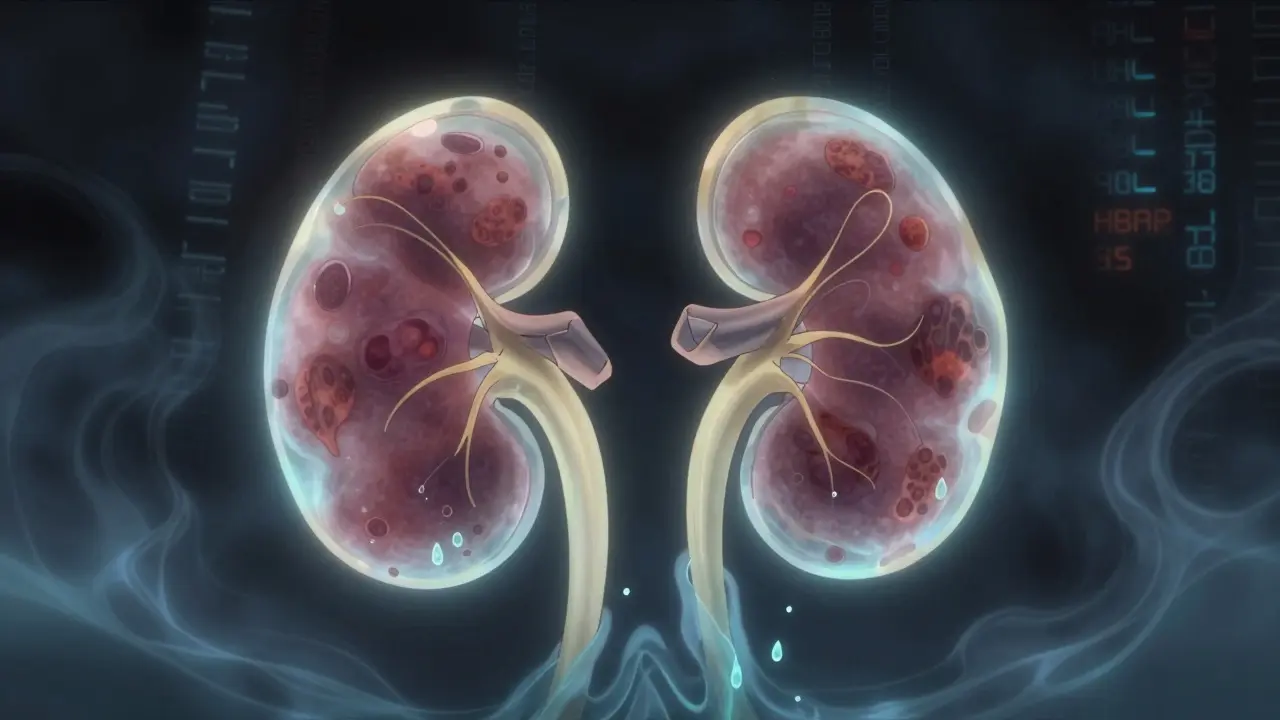
When your kidneys start leaking protein, it’s not just a lab result-it’s your body screaming for help. For people with diabetes, albuminuria is that early warning sign most miss. It’s not about feeling tired or swollen. It’s about a tiny amount of protein in your urine that shows your kidneys are already under attack. And if you ignore it, you’re not just risking kidney failure-you’re putting your heart at risk too.
What Albuminuria Really Means
Albuminuria isn’t a disease. It’s a signal. It means the filters in your kidneys-tiny structures called glomeruli-are damaged. In healthy kidneys, albumin, a protein your body needs, stays in your blood. But when high blood sugar wears down those filters, albumin slips through into your urine. That’s albuminuria.
The good news? It’s detectable long before you feel anything. The bad news? Most people don’t get tested until it’s too late. According to the American Diabetes Association, everyone with type 2 diabetes should get a urine test for albumin at diagnosis, and everyone with type 1 diabetes should be tested after five years. Yet, in real-world clinics, only about 60% of patients actually get this test done annually.
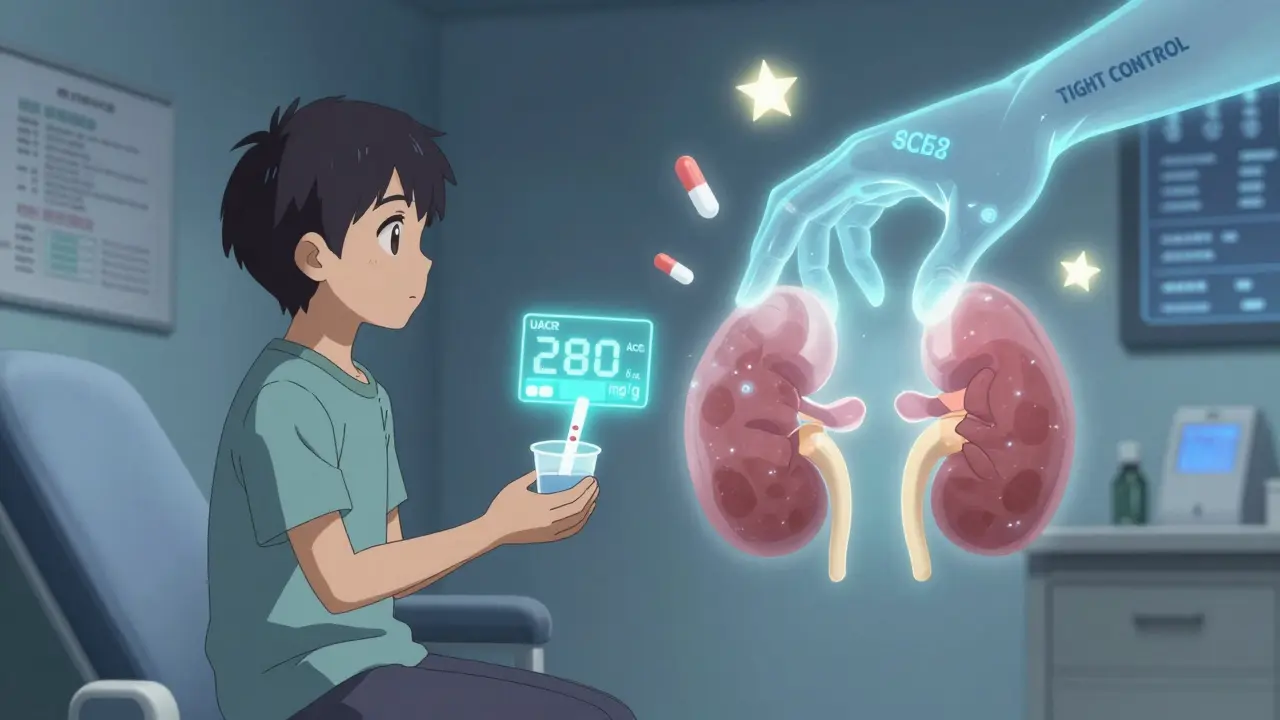
The test is simple: a spot urine sample that measures the albumin-to-creatinine ratio (UACR). Normal is under 30 mg/g. Anything above that? That’s kidney damage. KDIGO guidelines updated the terminology in 2012 to remove the word “micro” from microalbuminuria because even a little albumin matters. There are three levels:
- Normal: less than 30 mg/g
- Moderately increased: 30-300 mg/g
- Severely increased: over 300 mg/g
Here’s the catch: one high reading doesn’t mean you have diabetic kidney disease. Albuminuria can spike temporarily from a hard workout, an infection, high blood pressure, or even your period. That’s why guidelines say you need two out of three abnormal tests over three to six months to confirm it’s real.
Why Albuminuria Is the Best Early Warning System
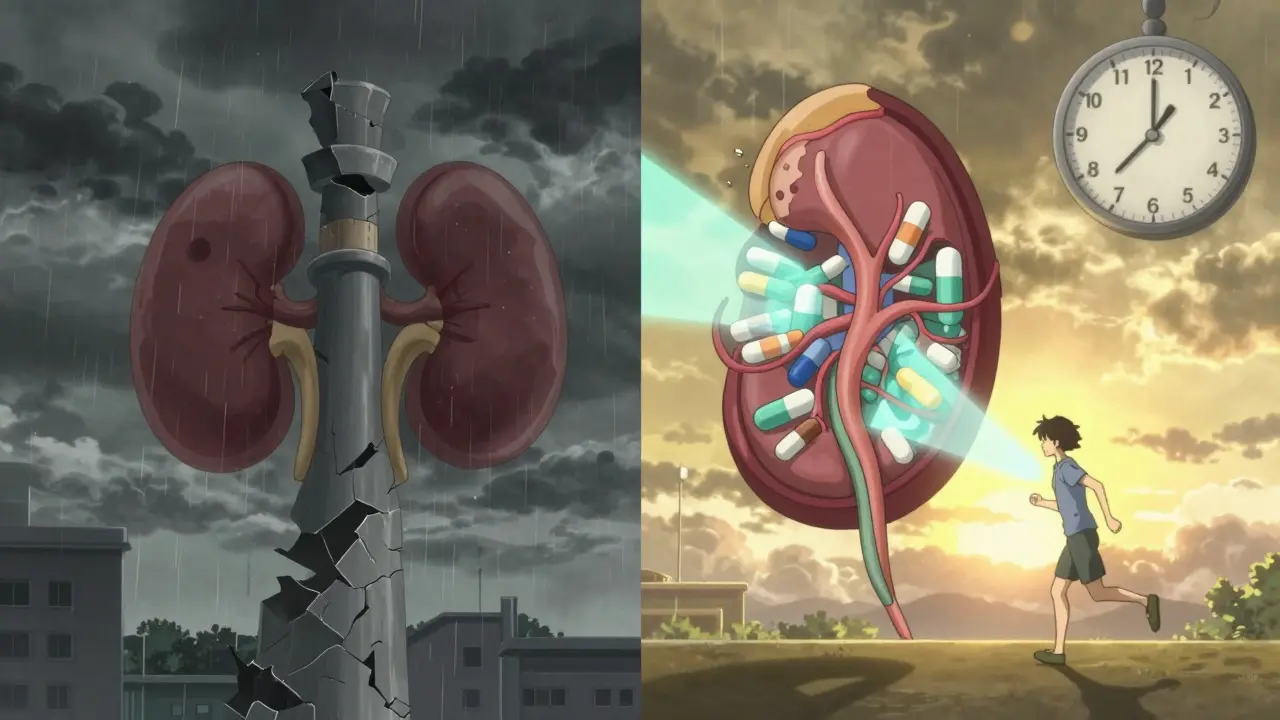
Think of albuminuria like a smoke detector. It goes off before the fire spreads. A 2021 analysis of over 128,000 diabetic patients showed that those with severely increased albuminuria (>300 mg/g) had a 73% higher risk of dying from any cause and an 81% higher risk of dying from heart disease compared to those with no albuminuria.
And here’s the kicker: the amount of albumin in your urine predicts your future. If your UACR climbs from 50 to 200 mg/g over a year, your kidneys are declining. If it drops from 250 to 80 mg/g after treatment, your kidneys are healing. That’s why doctors now track albuminuria not just to diagnose, but to measure how well treatment is working.
The landmark DCCT/EDIC study proved this. People with type 1 diabetes who kept their HbA1c below 7% for years cut their risk of developing microalbuminuria by 39% and proteinuria by 54%. Even more powerful? Those benefits lasted decades-even if their blood sugar later drifted up. That’s called “metabolic memory.” Your kidneys remember the good control.
For type 2 diabetes, the UKPDS study showed each 1% drop in HbA1c meant a 21% lower risk of kidney damage. That’s not a small win. That’s life-changing.
Tight Control Isn’t Just About Sugar
Many think tight control means only watching carbs. It doesn’t. It means hitting three targets: blood sugar, blood pressure, and cholesterol. And for kidney protection, blood pressure matters just as much.
KDIGO recommends aiming for under 120/80 mmHg if your albuminuria is above 300 mg/g. But the SPRINT trial showed that pushing systolic pressure below 120 mmHg reduced macroalbuminuria by 39%-but also increased the risk of acute kidney injury in 1 out of every 47 people. That’s why the ADA recommends a more practical target: under 140/90 mmHg for most people with diabetic kidney disease.
Medications make a huge difference. ACE inhibitors and ARBs (like lisinopril or losartan) aren’t just for blood pressure. They directly protect the kidneys by reducing pressure inside the filtering units. The IRMA-2 trial showed that giving losartan at the maximum dose (100 mg/day) to people with early albuminuria cut progression to severe proteinuria by 53%. And you don’t need high blood pressure to benefit-this works even if your pressure is normal.
But here’s where most clinics fail: they don’t titrate these drugs to the highest tolerated dose. A 2023 study found that only 38% of patients on ACE inhibitors or ARBs were on the full recommended dose. That’s like taking half a pill every day and wondering why it’s not working.
The New Game-Changers: SGLT2 Inhibitors and Finerenone
For years, ACE inhibitors and ARBs were the only drugs proven to slow diabetic kidney disease. Now, two new classes have joined the fight.
SGLT2 inhibitors-like empagliflozin, dapagliflozin, and canagliflozin-were originally designed to lower blood sugar by making your kidneys flush out glucose. But they do something even more powerful: they reduce pressure inside the kidney’s filtering units. The 2023 EMPA-KIDNEY trial showed that empagliflozin cut the risk of kidney failure or death from kidney disease by 28% in patients with UACR above 200 mg/g. And it didn’t just help people with high blood sugar-it worked even if they were already on an ACE inhibitor.
Then there’s finerenone. This newer drug blocks a hormone called aldosterone that causes scarring in the kidneys. In trials, it reduced albuminuria by 32% in just four months and slowed kidney function decline by 23% over three years-even when patients were already on maximum ACE/ARB therapy. It’s not a magic bullet, but it’s a powerful second layer of protection.
Yet, only about 29% of patients with diabetic kidney disease are getting both an SGLT2 inhibitor and an ACE/ARB. Why? Cost, confusion, fear of side effects, or simply no one ever told them these drugs exist for kidney protection.
The Real Problem: We’re Not Testing or Treating
Here’s the truth: we know exactly what to do. We have the tests. We have the drugs. We have the guidelines from ADA, KDIGO, and NKF-all aligned. So why is diabetic kidney disease still rising?
NHANES data from 2017-2018 showed that only 12.2% of U.S. adults with diabetes hit all three targets: HbA1c under 7%, blood pressure under 140/90, and LDL cholesterol under 100. In community clinics, UACR testing rates hover around 60%. Electronic health records rarely remind doctors to order it. Patients forget to collect urine samples. Providers don’t know how to interpret the results.
One study found that 78% of clinics said they lacked automated alerts in their systems. Another found that 23% of patients failed to return for a second test after an initial abnormal result. And 41% of primary care doctors didn’t realize albuminuria was a stronger predictor of kidney failure than HbA1c.
But some places are fixing it. University Hospitals in Ohio started using EHR alerts that pop up when a diabetic patient’s last UACR was over 30 mg/g. They added point-of-care urine testing in the exam room-no waiting for the lab. And they hired pharmacists to manage medication doses. Result? 89% of patients reached maximum tolerated ACE/ARB doses. That’s not luck. That’s system design.
What You Can Do Right Now
If you have diabetes, here’s your action list:
- Ask for your UACR result at your next visit. Don’t wait for your doctor to bring it up.
- If your result is above 30 mg/g, ask for two more tests over the next six months to confirm.
- If confirmed, ask if you’re on an ACE inhibitor or ARB-and if you’re on the highest safe dose.
- Ask if you’re a candidate for an SGLT2 inhibitor or finerenone. These aren’t just for blood sugar-they’re for kidney protection.
- Don’t let a high UACR scare you. It’s a sign you can act. Reduce it by 30% or more, and you cut your risk of kidney failure by nearly half.
And if you’re a caregiver, a nurse, or a family member-remind them. This isn’t about being perfect. It’s about being consistent. One test. One pill. One blood pressure check. Over time, those small steps add up to saved kidneys and saved lives.
It’s Not Too Late
Diabetic kidney disease isn’t inevitable. It’s not a slow march to dialysis. It’s a preventable chain reaction-and albuminuria is the first link. Catch it early. Treat it hard. And don’t stop until your UACR is back in the normal range.
The data is clear: tight control works. The tools exist. The guidelines are solid. What’s missing is action. Not from patients. Not from doctors. But from the system that lets too many people slip through the cracks.
Your kidneys don’t ask for much. Just a little attention. A simple test. A few pills. And the will to act before it’s too late.
What is the normal range for albumin in urine?
The normal range for albumin in urine is less than 30 mg per gram of creatinine (UACR). Anything above that-30 to 300 mg/g-is considered moderately increased albuminuria, and over 300 mg/g is severely increased. Even small amounts above 30 indicate early kidney damage in people with diabetes.
How often should people with diabetes get tested for albuminuria?
Everyone with type 2 diabetes should be tested at diagnosis. Everyone with type 1 diabetes should start annual testing after five years of diagnosis. If albuminuria is found, testing should continue every three to six months until it’s under control. Once stable, annual testing is still recommended.
Can albuminuria go away?
Yes, albuminuria can improve or even return to normal with proper treatment. Tight blood sugar control, blood pressure management with ACE inhibitors or ARBs, and newer medications like SGLT2 inhibitors and finerenone have all been shown to reduce albuminuria. In fact, a 30% or greater reduction in UACR is linked to a 48-56% lower risk of kidney failure.
Why do some doctors not test for albuminuria regularly?
Many clinics lack automated reminders in their electronic health records, and some providers aren’t fully aware of how predictive albuminuria is for kidney and heart disease. Patient non-adherence to urine collection and the misconception that albuminuria only matters if blood pressure is high also contribute to low testing rates-despite it being a Class A recommendation from the American Diabetes Association.
Do I need to take medication if my albuminuria is only slightly elevated?
Yes. Even moderately increased albuminuria (30-300 mg/g) signals early kidney damage and raises your risk of heart disease and kidney failure. Guidelines recommend starting an ACE inhibitor or ARB regardless of blood pressure level. These drugs protect your kidneys directly, not just by lowering pressure. Delaying treatment increases the chance of progression to more severe stages.
What’s the difference between SGLT2 inhibitors and ACE inhibitors for kidney protection?
ACE inhibitors and ARBs work by reducing pressure inside the kidney’s filtering units and blocking harmful hormones. SGLT2 inhibitors work differently-they cause the kidneys to excrete glucose and sodium, which lowers pressure and reduces inflammation. Both are protective, but they work through separate pathways. Current guidelines recommend using both together for maximum kidney protection in patients with albuminuria.
Can lifestyle changes alone reverse albuminuria?
Lifestyle changes-like losing weight, cutting salt, exercising, and controlling blood sugar-are essential. But for most people with diabetes and albuminuria, medication is needed to achieve meaningful reductions. Studies show that even with perfect lifestyle habits, albuminuria often persists without ACE inhibitors, SGLT2 inhibitors, or finerenone. The best results come from combining both.
Is albuminuria only a problem for people with type 1 diabetes?
No. While type 1 diabetes was studied first, type 2 diabetes causes far more cases of diabetic kidney disease because it’s much more common. In fact, most people with diabetic kidney disease have type 2. The same screening and treatment rules apply to both types. Albuminuria is the earliest sign in both.

14 Comments
Dwayne hiers
16 December, 2025Albuminuria is a glomerular filtration barrier dysfunction marker, not merely a lab anomaly. The UACR >30 mg/g threshold reflects podocyte injury and endothelial glycocalyx degradation-both driven by hyperglycemic flux and RAAS overactivation. Early intervention with ACEi/ARBs halts nephrin downregulation, and SGLT2i add tubuloglomerular feedback modulation. This isn’t speculative-it’s class I evidence from EMPA-KIDNEY and FIDELIO-DKD.
Sarthak Jain
16 December, 2025bro i just got my uacr back and its 87… i thought i was doing good with my diet but now i’m scared. is it too late? i’m on metformin but no other meds yet. anyone else in this boat?
Thomas Anderson
17 December, 2025Don’t panic. That number means your kidneys are telling you to pay attention, not that you’re doomed. Start the ACE inhibitor, get your BP under control, and move your butt. You’ve got time. I’ve seen people drop from 200 to 45 in a year with just meds and walking 10K steps a day.
Daniel Wevik
18 December, 2025That’s exactly right. The key is consistency-not perfection. SGLT2 inhibitors reduce intraglomerular pressure by 15–20%, independent of glucose control. That’s why even patients with HbA1c 8.5% benefit. And yes, the dose matters. Most docs leave patients on 5mg lisinopril when 40mg is the target. You’ve got to push for the full dose.
jeremy carroll
19 December, 2025just got my doc to put me on empagliflozin last month and my uacr dropped from 198 to 92 in 4 months. i didn’t even lose weight. i think this drug is magic. also my energy is way better. no more afternoon crashes. anyone else feel this?
Rich Robertson
20 December, 2025It’s wild how much we’ve learned in the last decade. Back in 2005, we thought if you had diabetes and your kidneys started failing, it was just fate. Now we know it’s a cascade-and we’ve got tools to break every link. ACEi, ARB, SGLT2i, finerenone… it’s like having a whole arsenal. The problem isn’t science. It’s access. People in rural clinics still don’t have urine dipsticks in the exam room. That’s the real crisis.
Natalie Koeber
21 December, 2025so… are you guys aware that the ADA gets funding from big pharma? like… why are they pushing all these drugs? what if albuminuria is just a side effect of modern processed food? what if we’re being sold a cure so they can keep selling meds? i mean… my grandma had diabetes in the 50s and never took a pill. she lived to 92.
Edward Stevens
23 December, 2025Wow. So we’re blaming processed food now? Next you’ll say insulin was invented by the Illuminati. Your grandma had no statins, no BP meds, no glucose monitors, and probably died of a heart attack at 70. You’re romanticizing ignorance. Also, the ADA guidelines are based on 128,000-patient trials, not ads on YouTube.
Rulich Pretorius
24 December, 2025There’s a deeper truth here: medicine has become transactional. We treat numbers, not people. The patient who gets tested once, then vanishes, isn’t failing because they’re lazy-they’re failing because the system doesn’t follow up. It’s not about willpower. It’s about design. If your EHR doesn’t ping you, you’re invisible. That’s the real epidemic.
Wade Mercer
24 December, 2025People need to stop treating diabetes like a hobby. It’s not ‘I’ll eat better next week.’ It’s a lifelong war against your own biology. If you’re not checking your urine, you’re not serious. And if you’re not on an ACE inhibitor by year one, you’re gambling with your kidneys. This isn’t a suggestion-it’s a moral obligation.
Sinéad Griffin
26 December, 2025FINERENONE IS A GAME CHANGER!!! 🚀 I’ve been on it 6 months and my albumin dropped 40%! My nephrologist said it’s like hitting the reset button on my kidneys. Also, no more leg cramps! 💪🩺 #DiabeticKidneyWarrior
Tim Bartik
27 December, 2025ok but why are we letting the feds tell us what to do? in america we don’t need some journal to tell us to take pills. my cousin in mexico just eats garlic and lemon water and his sugar’s perfect. why are we so weak? this whole system is broken. we need to go back to real food and real medicine.
Alexis Wright
28 December, 2025Let’s be brutally honest: albuminuria isn’t a medical problem-it’s a societal failure. We’ve created a population that’s chronically inflamed, sedentary, and medicated to the gills. We diagnose it, then we treat it with pharmaceuticals that cost $1,200/month. Meanwhile, the same system denies access to nutritionists, gym memberships, and mental health care. This isn’t healthcare. It’s profit-driven triage. The real question isn’t ‘how do we treat albuminuria?’ It’s ‘how do we stop creating it?’
Daniel Thompson
28 December, 2025As a nephrologist with 22 years of experience, I’ve seen patients reverse albuminuria from 450 to 25 mg/g. It’s not common, but it happens. The key? Multidisciplinary care: pharmacist-managed meds, dietitian-led low-sodium plans, and weekly BP logs. The magic isn’t in one drug-it’s in the system. And yes, I’ve seen patients who refused SGLT2i because they thought it was ‘too new’… and ended up on dialysis by 52. Don’t be that person.