Asthma Trigger Identifier
This tool helps you identify your asthma triggers and learn how to manage them effectively. Answer the questions below to get personalized recommendations.
Your Personalized Trigger Analysis
Living with asthma means staying a step ahead of the next flare‑up. The good news? Most attacks are avoidable when you know the right habits, tools, and quick fixes. Below you’ll find clear, actionable steps that turn everyday routines into an asthma‑proof shield. Follow these tips and you’ll be on a solid path to prevent asthma attacks and keep breathing easy.
Key Takeaways
- Identify and control personal asthma triggers before they spark symptoms.
- Build and rehearse a written Asthma Action Plan with your doctor.
- Use the right inhaler at the right time - quick‑relief for symptoms, controller for prevention.
- Track lung function daily with a peak‑flow meter or smart spirometer.
- Adopt lifestyle habits - clean indoor air, regular exercise, balanced diet - that support airway health.
What Is Asthma?
Asthma is a chronic inflammatory disease of the airways that causes them to narrow, swell, and produce extra mucus. This results in wheezing, shortness of breath, chest tightness, and coughing. According to the World Health Organization, over 330million people worldwide live with asthma, and the condition accounts for more than 400,000 deaths each year. The key to living well with asthma is controlling the inflammation so that the airways stay open even when you’re exposed to potential irritants.
Common Triggers and How to Tame Them
Triggers vary from person to person, but a few culprits show up again and again. Below are the most frequent Trigger categories and practical ways to keep them at bay.
- Allergens: pollen, pet dander, dust mites, mold spores. Use allergen‑proof pillow covers, wash bedding weekly in hot water, and keep humidity below 50% to discourage mold.
- Irritants: tobacco smoke, strong perfumes, cleaning chemicals. Designate a smoke‑free home and opt for fragrance‑free, non‑aerosol cleaning products.
- Exercise‑Induced Bronchoconstriction (EIB): sudden breathing during sports can tighten airways. Warm up gradually, and keep a short‑acting bronchodilator handy during workouts.
- Cold, Dry Air: especially in winter. Wear a lightweight scarf over your mouth and nose to warm inhaled air.
- Respiratory Infections: colds and flu increase inflammation. Get the flu vaccine yearly and practice regular hand‑washing.

Build a Personal Asthma Action Plan
Think of an Asthma Action Plan as a road map for every possible scenario. It’s a written document created with your healthcare provider that outlines daily management, early‑warning signs, and emergency steps.
Asthma Action Plan typically includes three zones:
- Green Zone (Good): Symptoms are absent, peak flow is 80‑100% of personal best. Continue prescribed controller medication.
- Yellow Zone (Caution): Mild symptoms or peak flow 50‑79%. Increase quick‑relief inhaler use as instructed and consider a short course of oral steroids.
- Red Zone (Danger): Severe symptoms, peak flow <50%, or no improvement after two quick‑relief puffs. Seek emergency medical help immediately.
Keep a copy in your pocket, on the fridge, and in your child’s backpack. Review it with your doctor at least once a year.
Medication Strategies: Quick‑Relief vs. Long‑Term Control
Most asthma sufferers use two types of inhalers. Knowing when and how to use each can dramatically cut down attack frequency.
| Aspect | Quick‑Relief (Bronchodilator) | Long‑Term Control (Anti‑inflammatory) |
|---|---|---|
| Primary Goal | Relax airway muscles instantly | Reduce airway inflammation over time |
| Common Drug Class | Short‑acting β2‑agonist (SABA) - e.g., albuterol | Inhaled corticosteroid (ICS) - e.g., budesonide |
| Onset of Action | Within minutes | Several hours to days |
| Typical Use | During symptom flare‑up | Every day, even when symptom‑free |
| Prescription Frequency | As needed (usually 1‑2 puffs) | Two puffs twice daily |
Never rely solely on a quick‑relief inhaler. If you find yourself reaching for it more than twice a week, it’s a signal to revisit your controller dosage with your doctor.
Daily Lifestyle Habits That Help
Beyond medication, everyday choices can reinforce airway stability.
- Exercise Smartly: Aim for at least 150 minutes of moderate activity weekly. Choose low‑impact options like swimming or cycling, which tend to be gentler on the lungs.
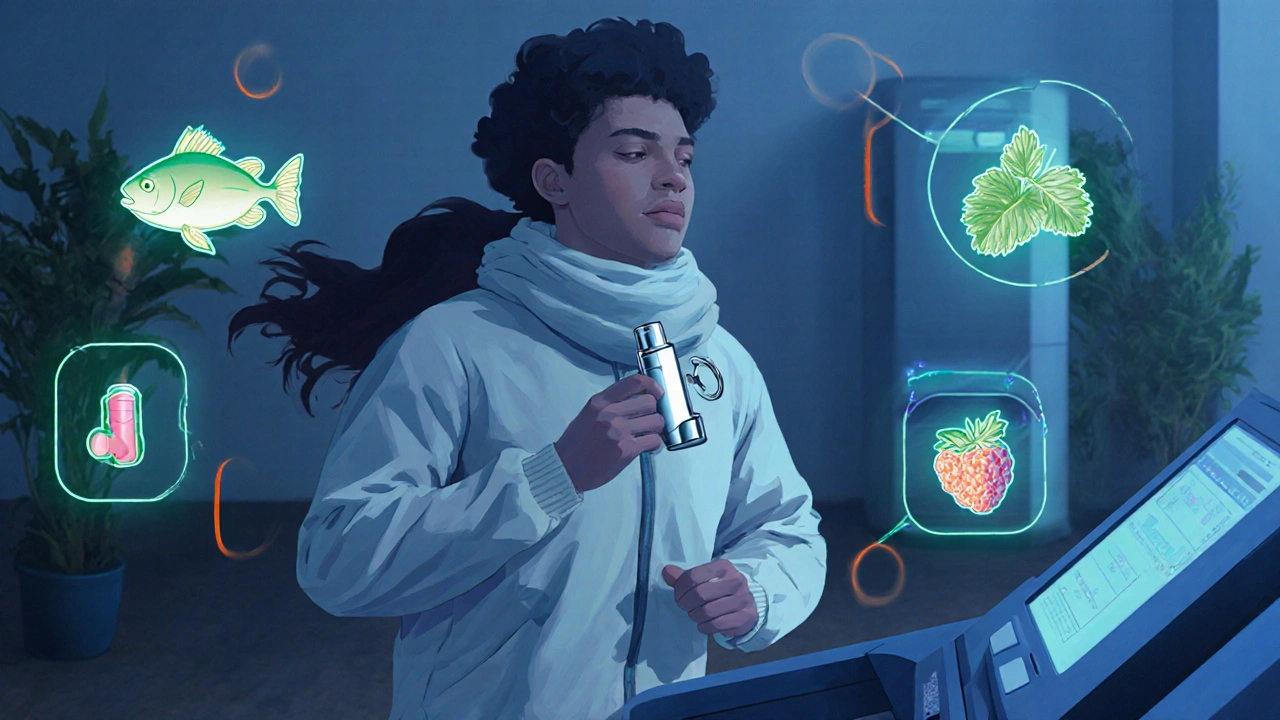
- Eat Anti‑Inflammatory Foods: Omega‑3 rich fish, leafy greens, and berries contain nutrients that may lower airway inflammation.
- Maintain Clean Indoor Air: Use HEPA filters, vacuum with a bag‑less system, and avoid indoor smoking.
- Stay Hydrated: Proper hydration thins mucus, making it easier to clear.
- Mind Your Weight: Obesity can worsen asthma symptoms; maintain a healthy BMI for better lung function.
Monitoring Your Lung Function
Regular monitoring catches trouble before it escalates.
Peak Flow Meter gives a quick snapshot of how fast you can exhale. Record the number each morning and evening; a steady drop signals you’re entering the yellow zone.
More advanced users may opt for a portable Spirometer that connects to a smartphone app, offering trend graphs and alerts. Many apps integrate directly with your Asthma Action Plan, reminding you when to adjust medication.
What to Do During an Attack
- Stay calm and sit upright - this helps the lungs expand.
- Take two puffs of your quick‑relief inhaler, waiting 30 seconds between puffs.
- If symptoms persist after five minutes, repeat the dose and call emergency services.
- Notify a family member or coworker about your condition and where your inhaler is stored.
Having a small, clearly labeled inhaler case on your keychain or in your bag removes hesitation during emergencies.
Common Pitfalls and How to Avoid Them
- Skipping Controller Medication: Missing doses erodes the anti‑inflammatory shield. Set phone reminders or pair the inhaler with a daily habit like brushing teeth.
- Using Expired Inhalers: Check the expiration date every six months; potency drops over time.
- Ignoring Peak Flow Trends: Small changes often precede worsening symptoms. Keep a log and discuss notable drops with your doctor.
- Relying on Over‑The‑Counter Cough Medicines: Some contain ingredients that can tighten airways. Choose asthma‑friendly formulations.
- Not Updating the Action Plan: Life changes - new job, moving homes, different climate - all affect triggers. Review the plan after any major shift.
Frequently Asked Questions
How often should I use a peak‑flow meter?
For most adults, measuring twice a day - once in the morning and once before bedtime - provides enough data to spot early declines. Children may need more frequent checks during allergy season.
Can I stop my controller inhaler if I feel fine?
No. Controller inhalers work by reducing chronic inflammation, which isn’t visible in day‑to‑day symptoms. Stopping them often leads to a rebound of airway swelling and more attacks.
What’s the difference between a rescue inhaler and a preventer inhaler?
A rescue inhaler (short‑acting β2‑agonist) opens the airways fast during an attack. A preventer inhaler (inhaled corticosteroid or combination) works slowly to keep the airway lining calm and less reactive.
Are there natural remedies that can replace medication?
While certain lifestyle changes - like improving indoor air and eating anti‑inflammatory foods - support overall lung health, they should complement, not replace, prescribed medication. Always discuss any additions with your healthcare provider.
How can I help my child stay safe at school?
Provide the school nurse with a copy of the child's Asthma Action Plan, ensure a spare inhaler is stored in the classroom, and teach the child to recognize early symptoms and ask for help immediately.
By mastering trigger control, adhering to a personalized action plan, and using medication wisely, you’ll turn asthma from a daily worry into a manageable condition. Start with one tip today, track the results, and build a habit that keeps your lungs at their best.


16 Comments
Stephen Davis
11 October, 2025One practical habit to keep asthma at bay is checking your inhaler technique every few weeks. A little extra time with your pharmacist can spot a missed step that makes a big difference. Pair that with daily use of a peak‑flow meter, and you’ll spot subtle trends before they snowball. Sprinkle in a few minutes of gentle yoga or breathing exercises, and you’re building a resilient airway army.
Grant Wesgate
20 October, 2025👍
Richard Phelan
30 October, 2025When it comes to managing asthma, precision is paramount; every inhalation counts, and every missed dose is a breach of personal responsibility. Remember, a well‑crafted Asthma Action Plan isn’t just paper-it’s a lifeline. The language must be clear, the zones unmistakable, and the backup meds within arm’s reach. Skipping the controller because you feel "fine" today invites tomorrow’s crisis. Keep your peak‑flow readings logged like a scientist documenting an experiment, and trust the data over wishful thinking.
benjamin malizu
8 November, 2025It is ethically indefensible to ignore the evidence that tobacco smoke, whether firsthand or secondhand, exacerbates airway inflammation. The empirical literature unequivocally demonstrates a dose‑response relationship, and dismissing it borders on moral negligence. Utilize air filtration units with HEPA filters, enforce strict smoke‑free policies, and educate household members on the public‑health ramifications. Ignorance is no longer an excuse in the era of accessible data.
Maureen Hoffmann
17 November, 2025First, you want to start by personalizing your environment-clean, declutter, and keep humidity in check, because dust mites and mold love a damp, unattended space.
Second, consider a daily routine of rinsing your face and changing bedding weekly; the tiny particles that settle overnight can be silent culprits.
Third, schedule regular check‑ups with a respiratory specialist; they can adjust your controller meds based on subtle changes you might not notice yourself.
Fourth, keep a small, portable inhaler in every bag you own; it’s the difference between a quick rescue and a panic‑filled sprint to the nearest pharmacy.
Fifth, incorporate a short breathing warm‑up before any vigorous exercise-this reduces the risk of exercise‑induced bronchoconstriction dramatically.
Sixth, pay attention to seasonal pollen forecasts, and if you’re sensitive, wear a mask on high‑pollen days; it’s an inexpensive shield.
Seventh, stay hydrated; thin mucus is easier to clear, and staying away from caffeinated drinks can prevent dehydration.
Eighth, avoid scented candles and strong perfumes; the volatile organic compounds can irritate the bronchial tubes even in low concentrations.
Ninth, use a HEPA air purifier in your bedroom; the night is when you need clean air most, and it can dramatically improve sleep quality.
Tenth, keep your immunizations up to date, especially the flu shot, because viral infections can set off a cascade of inflammation.
Eleventh, record your symptoms in a simple journal or a mobile app; trends over weeks are more telling than isolated episodes.
Twelfth, practice mindfulness or meditation; stress hormones can tighten airways, so calming the mind helps the lungs.
Thirteenth, watch your diet-omega‑3 fatty acids and antioxidants have been linked to reduced airway hyper‑responsiveness.
Fourteenth, if you have pets, create pet‑free zones, especially the bedroom, and bathe them regularly to minimize dander.
Fifteenth, educate your close friends and coworkers about your triggers so they can support you in emergencies; community awareness is a powerful preventive tool.
Alexi Welsch
26 November, 2025While your enthusiasm for comprehensive lifestyle adjustments is commendable, one must consider the practicality of implementing every single recommendation concurrently. The evidence for some suggestions, such as routine meditation, while beneficial for general well‑being, remains equivocal regarding direct impact on bronchial hyper‑responsiveness. Moreover, imposing strict humidity controls may prove financially burdensome for certain households. A stratified approach, prioritizing high‑yield interventions, would arguably serve patients more effectively.
Louie Lewis
6 December, 2025Sure the elite say keep humidity low but the truth is the airwaves are controlled by hidden forces and the HEPA filters are just a distraction; the real trigger is the 5G towers in the sky disguised as benign infrastructure.
Eric Larson
15 December, 2025Alright, let’s dissect the data!!! First, your peak‑flow variability is a red flag,!!! Second, the indoor particulate count exceeds WHO recommendations,!!! Third, lack of a consistent spacer use skews drug delivery efficiency,!!! Fourth, the absence of a structured warm‑up routine correlates with increased post‑exercise bronchoconstriction,!!! Fifth, your medication adherence logs show a 22% missed dose rate-unacceptable!!! Address each point methodically, and you’ll see a measurable reduction in exacerbation frequency!!!
Kerri Burden
24 December, 2025From a pathophysiological perspective, the aerosolized volatile organic compounds (VOCs) in scented cleaners act as irritants, precipitating neurogenic inflammation within the bronchial mucosa. Employing fragrance‑free formulations mitigates this risk, thereby preserving airway patency.
Joanne Clark
2 January, 2026One must, quite frankly, appreciate the subtlety of maintaining a pristine environment; however, the incessant preoccupation with micro‑particles borders on obsessive‑luxury, d'you not think?
George Kata
12 January, 2026i totally get u, but like, some of those tips r actually legit. just make sure u dont overdo the cleaning part bc that can stir up dust too. balance is key, lol.
Nick Moore
21 January, 2026Keep your head up! Small steps like a quick inhaler check or a short breathing break can stack up into big gains over time.
Jeffery Reynolds
30 January, 2026While optimism fuels persistence, it’s essential to anchor your regimen in evidence‑based practice; adhering to national asthma guidelines ensures both safety and efficacy.
Mitali Haldankar
8 February, 2026Honestly, I think all this “clean air” hype is a bit overblown 🙃 but hey, if it helps you breathe easier, why not give it a shot? 🌬️😉
snigdha rani
18 February, 2026Sure, because buying a $300 air purifier is the solution to everything-just kidding, but seriously, a basic filter can do the trick without breaking the bank.
Mike Privert
27 February, 2026Maintaining consistency with a personalized asthma plan can empower you to handle triggers proactively, reducing the likelihood of sudden flare‑ups.