For years, rheumatoid arthritis (RA) was treated like a slow-burning fire-manage the symptoms, hope for the best, and accept that joint damage was just part of the deal. But that’s not how it works anymore. Today, remission isn’t a lucky break; it’s a realistic goal-and there’s a proven system to get there: treat-to-target (T2T).
What Treat-to-Target Really Means
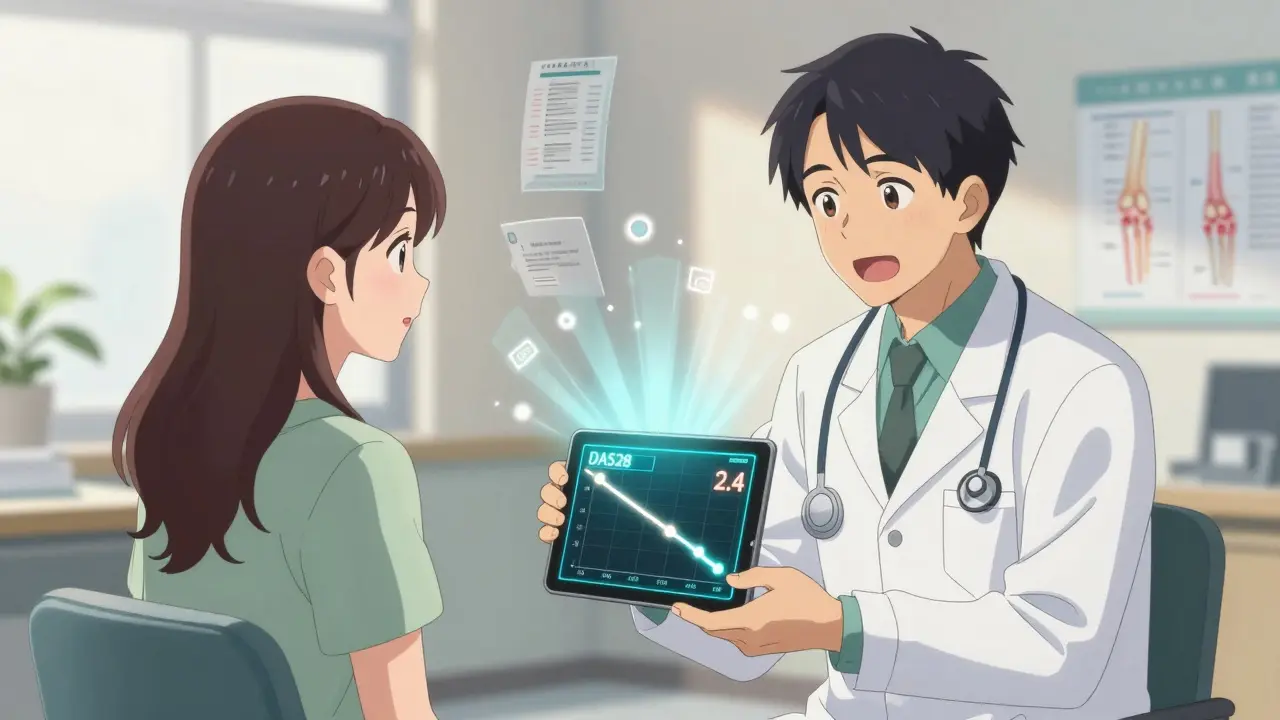
Treat-to-target isn’t a new drug. It’s not even a new idea. It’s a simple shift in how doctors and patients think about RA. Instead of waiting until pain gets worse before changing treatment, T2T says: Set a clear goal, check progress often, and adjust fast if you’re not hitting it. The goal? Remission-or at least low disease activity. The most common way to measure this is the DAS28 score. It counts swollen and tender joints, adds in blood markers like CRP or ESR, and gives you a number. If it’s below 2.6? You’re in remission. Between 2.6 and 3.2? You’re in low disease activity. Simple. Objective. No guesswork. This approach was proven in real-world studies like the DREAM trial in the Netherlands, where nearly 60% of early RA patients reached remission after a year using T2T. Compare that to traditional care, where only about 30% got there. That’s not a small difference-it’s life-changing.How T2T Works Step by Step
Here’s how it actually plays out in a clinic:- Start with a baseline. Your rheumatologist measures your DAS28, checks for joint damage on X-rays or ultrasounds, and asks how you’re feeling day-to-day.
- Set the target. Remission? Or just low disease activity? This isn’t one-size-fits-all. Some patients want to get off steroids. Others just want to hold onto their job. The goal is personalized.
- Start treatment. Most people begin with methotrexate-usually 15-25 mg a week. It’s cheap, well-studied, and works for many.
- Check in every 1-3 months. If your DAS28 hasn’t dropped by at least 1.2 points in 3 months? You’re not on track. Time to adjust.
- Step up if needed. If methotrexate alone isn’t enough, doctors add another DMARD-like sulfasalazine or hydroxychloroquine-to make triple therapy. If that still doesn’t work, biologics or JAK inhibitors come in: adalimumab, tocilizumab, baricitinib, etc.
- Keep going until you hit the target. Once you’re in remission, visits slow to every 3-6 months. But you don’t stop monitoring. Remission can slip away if you’re not careful.
What Works Best-And What Doesn’t
T2T shines brightest in early RA. If you’ve had symptoms for less than a year, your chances of hitting remission jump dramatically. That’s why catching RA early matters so much. But what if you’ve had it for 10 years? Studies show T2T still helps, but remission becomes harder. In established RA, the goal often shifts from full remission to low disease activity. That’s not failure-it’s progress. One patient I spoke with had been in pain for 15 years. She didn’t get to remission, but her DAS28 dropped from 5.8 to 2.9. She went from needing help to get out of bed to walking her dog every morning. That’s a win. The problem? Not every doctor uses T2T consistently. A 2022 study found that while 80% of rheumatologists say they aim for remission, only 41% actually set a clear target with their patients. And if you’re not measuring your DAS28 every few months, you’re not doing T2T-you’re just doing regular visits.
Why Patients Love It (When It’s Done Right)
On patient forums like CreakyJoints and MyRheumaTeam, people who’ve experienced true T2T talk about it like a revolution. “I was told I’d be in a wheelchair by 40,” wrote one user on Reddit in March 2023. “My new rheumatologist started checking my DAS28 every 6 weeks. I hit remission in 6 months. I’m 38 and hiking now.” That’s not an outlier. The Arthritis Foundation’s 2021 survey showed that 68% of patients on T2T reported better disease control, compared to just 42% on standard care. Satisfaction? 73% vs. 52%. But here’s the catch: if your doctor says they use T2T but only checks your CRP once a year, you’re being misled. Real T2T means regular, objective tracking. If you’re not getting scored at every visit, ask why.The Real Barriers
T2T sounds perfect. So why isn’t everyone doing it? First, time. Measuring 28 joints, calculating scores, adjusting meds-it takes longer than writing a prescription and saying “come back in 6 months.” Many clinics don’t have the staff or systems to support it. Second, access. Biologics and JAK inhibitors are expensive. In low-income countries, only 25% of RA patients can even get these drugs. T2T can’t work without the tools. Third, mindset. Some patients feel guilty if they don’t hit remission. “I followed everything,” one person wrote, “but my DAS28 stayed at 3.1. I felt like a failure.” That’s the dark side of targets. Not everyone can reach remission-and that’s okay. The goal isn’t perfection. It’s progress. Sometimes, the best outcome is staying off steroids, avoiding joint replacements, or being able to hold your grandchild without pain.What’s Next? Digital Tools and Personalized T2T
The future of T2T is getting smarter. Apps are now being tested that let patients log pain, stiffness, and fatigue daily. Wearables track movement and swelling. Algorithms combine that with blood test results to predict flare-ups before they happen. The DART trial in Australia is testing a smartphone app that sends alerts to doctors when a patient’s symptoms worsen. No waiting for the next appointment. Treatment adjusts in real time. Even more exciting? Research is starting to use genetics and protein markers to predict who will respond to which drug-before they even start. Imagine knowing, before your first injection, that tocilizumab will work for you and adalimumab won’t. That’s the next frontier.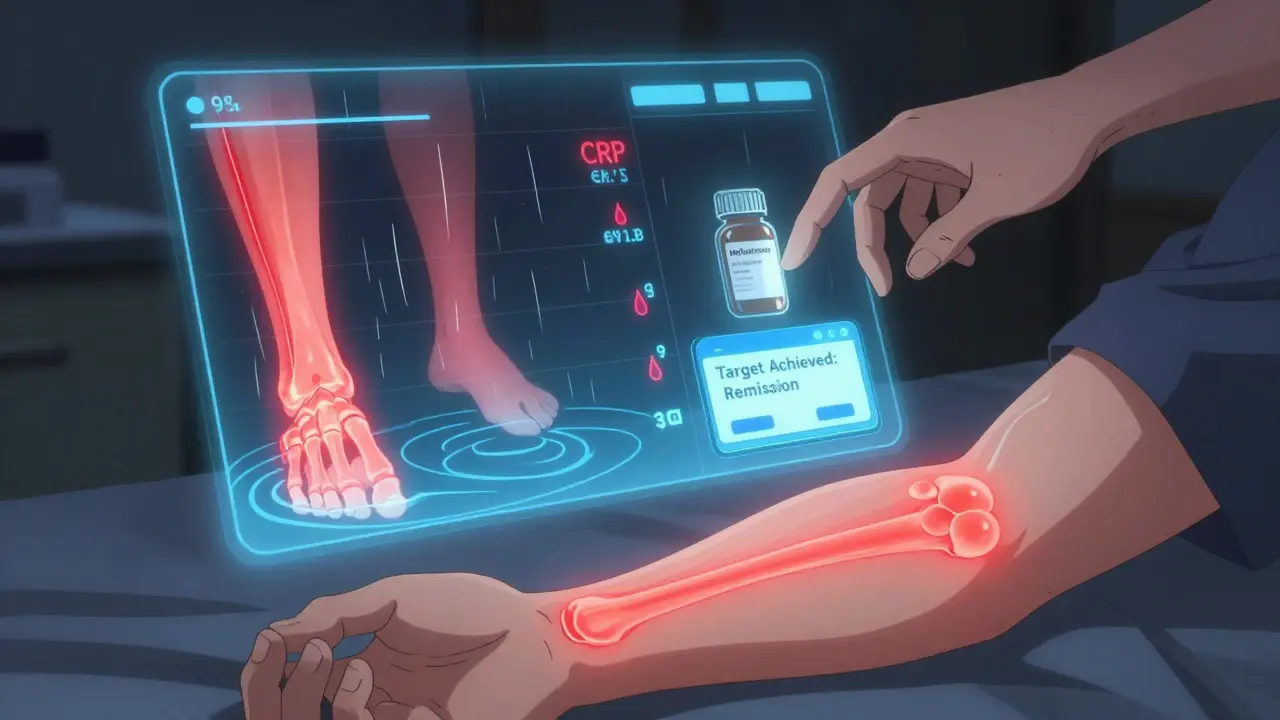
What You Can Do Today
You don’t need a fancy app or a research trial to start benefiting from T2T. Here’s how to take control:- Ask your rheumatologist: “What’s my DAS28 score right now? What’s our target?”
- Request a written treatment plan with clear milestones: “If my score doesn’t drop by X in 3 months, we’ll move to Y.”
- Track your own symptoms. Use a notebook or a free app like MyTherapy or Arthritis Power.
- If your doctor refuses to measure your disease activity regularly, consider finding one who does. Your joints will thank you.
- Remember: Remission isn’t the only win. Less pain, fewer flares, and staying off steroids count too.
Frequently Asked Questions
Can you really achieve remission with rheumatoid arthritis?
Yes. Multiple large studies, including DREAM, BeSt, and TICORA, show that 50-60% of early RA patients can reach remission using treat-to-target strategies. Even in long-standing RA, many achieve low disease activity, which significantly reduces joint damage and improves quality of life.
What’s the difference between remission and low disease activity?
Remission means almost no disease activity-DAS28 under 2.6. You might still have mild stiffness, but no swelling, no fatigue, and no joint damage progression. Low disease activity (DAS28 2.6-3.2) means some symptoms remain, but they’re controlled enough that daily life isn’t severely limited. Both are successful outcomes.
How often should I get my disease activity checked?
Every 1-3 months while your disease is active or you’re adjusting treatment. Once you’re stable in remission or low disease activity, every 3-6 months is standard. More frequent checks aren’t needed unless symptoms return.
Are biologics necessary for treat-to-target?
Not always. Many people reach remission with methotrexate alone or triple therapy (methotrexate + sulfasalazine + hydroxychloroquine). Biologics or JAK inhibitors are added if those don’t work after 3-6 months. They’re not a first-line requirement.
What if I can’t afford biologics?
Treat-to-target still works with conventional DMARDs. Studies show patients on methotrexate and combination therapy can reach remission, especially when monitored closely. Talk to your doctor about patient assistance programs, generics, or clinical trials. Don’t assume biologics are your only option.
Can I stop taking meds if I’m in remission?
Some people can reduce or stop meds under close supervision-but never on your own. Stopping too soon leads to flares in most cases. Even in remission, regular monitoring is essential. Many patients stay on low-dose methotrexate long-term to stay in remission.
Is T2T only for people with early RA?
No. While early RA responds best, T2T helps anyone with active disease. Even patients with 10+ years of RA can improve significantly-reducing pain, slowing damage, and avoiding surgery. The goal might shift from remission to low disease activity, but the strategy still works.

13 Comments
Jane Lucas
28 December, 2025i just started methotrexate last month and my joints dont feel like theyre made of glass anymore. thank you for this.
no more crying in the shower.
dean du plessis
29 December, 2025this is the first time i've read something about RA that actually made sense. no jargon, no fearmongering. just facts.
im printing this out for my doc.
Gerald Tardif
30 December, 2025you know what kills me? doctors who say they do T2T but only check CRP once a year. thats not a target, thats a suggestion.
youre not treating arthritis, youre just hoping it goes away.
John Barron
31 December, 2025The treat-to-target paradigm is not merely a clinical protocol; it is a paradigmatic shift in the epistemological framework of rheumatologic care, grounded in evidence-based medicine and operationalized through standardized disease activity indices such as DAS28. The DREAM and BeSt trials represent landmark studies that have redefined the therapeutic horizon for rheumatoid arthritis, demonstrating statistically significant improvements in remission rates when compared with traditional, symptom-driven management strategies. Furthermore, the integration of objective biomarkers such as CRP and ESR into routine clinical decision-making constitutes a necessary evolution away from subjective patient-reported outcomes alone. It is imperative that clinicians adopt this model with fidelity, as deviations from protocol-such as infrequent monitoring or failure to escalate therapy-undermine the very foundation of precision medicine in rheumatology.
Alex Lopez
2 January, 2026oh wow, so you're telling me if i actually go to the doctor and they measure my joints instead of just nodding and handing me a prescription... i might not be in a wheelchair by 40?
mind blown. 🤯
Miriam Piro
3 January, 2026they don't want you to know this.
the pharmaceutical companies are pushing biologics because they make billions.
they don't want you to know that methotrexate + sulfasalazine + hydroxychloroquine works just as well.
they want you dependent on $20,000/year drugs.
the DAS28 score? a tool to keep you coming back.
remission? a myth sold to keep you hopeful.
they're hiding the truth: RA is caused by glyphosate in your food and 5G radiation.
the FDA won't tell you because they're in bed with Big Pharma.
your doc doesn't want you to know because they get kickbacks.
ask yourself: why are there no long-term studies on natural cures?
because they can't patent turmeric.
you're being manipulated.
and if you're not checking your CRP every 2 weeks, you're not even trying. 🕵️♀️
Paula Alencar
5 January, 2026I want to extend my deepest gratitude to the author of this post-not merely for the clinical precision, but for the profound humanity embedded in every paragraph. So many of us with chronic illness have been gaslit by a medical system that treats our pain as anecdotal, our fatigue as laziness, our remission as a miracle rather than a measurable outcome. To see the DREAM and TICORA trials referenced with such clarity is to feel seen. And to those who say, 'I didn’t reach remission, so I failed'-please hear this: you did not fail. You fought. You tracked. You persisted. And that, in itself, is a victory that no score can diminish. Your dignity is not contingent on a number. Your worth is not measured in swollen joints. You are more than your disease. And you deserve every ounce of hope this approach offers.
Monika Naumann
5 January, 2026In India, we have no access to these biologics. Yet we still treat RA with traditional Ayurvedic herbs and strict dietary protocols. Why are you so focused on Western medicine? Our ancestors healed for centuries without DAS28 scores. This is cultural imperialism disguised as science.
Elizabeth Ganak
5 January, 2026i read this and cried. not because i'm sad, but because i finally feel like someone gets it.
my doc checks my joints every 6 weeks now.
i'm not in remission yet but i can pick up my kid again.
that's everything.
Raushan Richardson
6 January, 2026i used to think RA meant giving up on life. now i know it just means getting smarter about how you fight it.
my DAS28 dropped from 5.4 to 2.8 in 4 months.
not because i’m special. because i asked the right questions.
you can do this too.
you’re not broken. you’re just undiagnosed.
Satyakki Bhattacharjee
8 January, 2026people think science will save them. but truth is, suffering is the only real teacher.
your joints will rot. your body will betray you.
remission is just a pause before the next storm.
you think measuring DAS28 changes fate? it doesn't. it just makes you feel better about dying slower.
Liz MENDOZA
9 January, 2026thank you for writing this. i shared it with my sister who’s been told for 8 years that her pain is 'all in her head'.
she finally went back to her doctor.
they started her on methotrexate last week.
she cried when she told me she could tie her shoes without help.
you changed her life.
Kishor Raibole
11 January, 2026While the treat-to-target methodology presents a compelling framework grounded in empirical data, one must critically interrogate the underlying assumptions of biomedical hegemony. The conflation of disease activity with human value, the quantification of suffering through numerical indices, and the implicit hierarchy of 'remission' as the sole legitimate outcome-these are not neutral clinical practices, but ideological constructs embedded within capitalist healthcare systems. To equate remission with success is to erase the lived reality of those who persist in low disease activity, who endure chronic pain without collapse, who find meaning beyond the metric. The true revolution lies not in adjusting biologics, but in dismantling the very notion that a human being’s worth can be measured by a joint count.