When your kidneys aren’t working well, even common medicines can turn dangerous. A simple headache pill like ibuprofen might send your creatinine levels soaring. A diabetes drug you’ve taken for years could become toxic. This isn’t scare tactics-it’s clinical reality. One in seven Americans has chronic kidney disease (CKD), and medication errors are one of the top reasons people with CKD end up in the hospital. The good news? Most of these errors are preventable. You don’t need to be a doctor to understand the basics. You just need to know what to ask, what to avoid, and when to double-check.
Why Kidneys Change How Medicines Work
Your kidneys don’t just make urine. They filter your blood, removing waste and excess drugs. When kidney function drops, those drugs build up. That’s why a standard dose of a painkiller or antibiotic might be fine for someone with healthy kidneys but could poison someone with stage 3 CKD. The key number here is eGFR-estimated glomerular filtration rate. It tells you how well your kidneys are filtering. Once eGFR falls below 60 mL/min/1.73 m², most drugs cleared by the kidneys need a dose change. Below 30? Many need to be stopped entirely.It’s not just about quantity-it’s about timing. Some drugs, like gentamicin, are given once a day in CKD instead of every 8 hours. Others, like vancomycin, need their blood levels checked regularly. In healthy people, trough levels might be 15-20 mcg/mL. In someone with CKD not on dialysis? It’s 10-15 mcg/mL. Miss that, and you risk hearing loss, nerve damage, or worse.
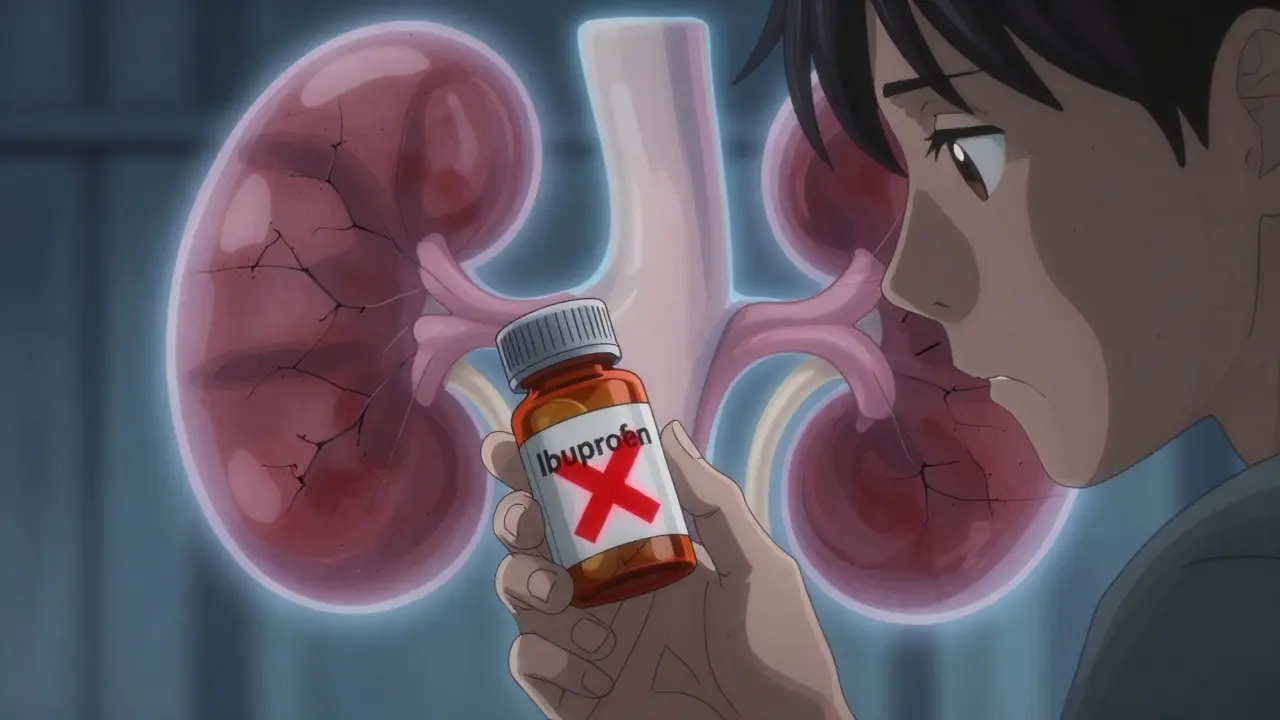
The Big Nephrotoxins You Need to Avoid
Some drugs are known to directly damage kidneys. These are called nephrotoxins. The most common ones? Nonsteroidal anti-inflammatory drugs (NSAIDs). That includes ibuprofen, naproxen, and even high-dose aspirin. They reduce blood flow to the kidneys. In someone with CKD, that can trigger acute kidney injury in under 48 hours. One patient on a kidney forum described taking two Advil for a headache-his creatinine jumped from 3.2 to 5.7. He ended up hospitalized.Other dangerous drugs include:
- Contrast dye used in CT scans-ask your doctor if you need a special protocol or hydration plan.
- Sodium phosphate bowel prep for colonoscopies-switch to PEG-based solutions instead.
- Some antibiotics like aminoglycosides (gentamicin, tobramycin) and certain antivirals.
- Herbal supplements like aristolochic acid (found in some traditional remedies)-linked to kidney failure and cancer.
Even OTC meds can be risky. Cold medicines often contain NSAIDs or pseudoephedrine, which can raise blood pressure and strain kidneys. Always check labels. If you’re unsure, ask your pharmacist. A 2023 NIDDK study found 68% of CKD patients didn’t know which over-the-counter drugs were unsafe.
Diabetes Medications: What’s Safe, What’s Not
People with CKD often have diabetes. Managing both is tricky. Metformin, once the go-to for type 2 diabetes, is now off-limits if eGFR is below 30. Between 30 and 45, use it with caution. The risk? Lactic acidosis-a rare but deadly buildup of acid in the blood.Here’s what’s changed: SGLT2 inhibitors like dapagliflozin and empagliflozin are now first-line. Why? They don’t need dose adjustments, even if your eGFR drops to 15. They also protect your kidneys. The CREDENCE trial showed they cut the risk of kidney failure or death by 39%. That’s not a small win-it’s life-changing. And you don’t even need to have diabetes to benefit. The 2024 KDIGO guidelines now recommend them for all CKD patients with albuminuria, regardless of blood sugar.
On the flip side, avoid sulfonylureas like glipizide or glyburide. They cause low blood sugar, and when kidneys can’t clear them, the risk skyrockets. You might feel dizzy, sweaty, confused-then pass out. It’s not worth the gamble.
ACE Inhibitors and ARBs: Don’t Underdose
For years, doctors held back on ACE inhibitors (like lisinopril) and ARBs (like losartan) in CKD patients. Why? Because they raise serum creatinine-a sign of reduced kidney blood flow. Many thought that meant harm.That thinking is wrong. The 2024 KDIGO guidelines say: maximize the dose. Even if creatinine rises by 30%, don’t stop. That rise isn’t damage-it’s the drug working. Clinical trials proving these drugs slow kidney disease used maximum tolerated doses. Lower doses? They don’t protect. One nephrologist put it bluntly: “Not using full doses out of fear of creatinine rise is suboptimal care.”
And now there’s a new player: finerenone. If you’re on an ACE/ARB and still have high urine albumin (over 30 mg/g), and your potassium is under 4.8 mmol/L, finerenone can be added. It’s not a replacement-it’s an upgrade. It cuts kidney and heart risks even further.
How to Stay Safe: Practical Steps
You can’t rely on your doctor to catch every mistake. Here’s what you can do:- Get your eGFR checked every 3-6 months. If it drops, review all your meds.
- Use one pharmacy. Studies show a 42% drop in medication-related kidney injuries when all prescriptions go through one place. Pharmacists can flag dangerous combinations.
- Ask: “Is this safe for my kidneys?” Every time a new drug is prescribed-even a short-term one.
- Carry a medication list. Include doses, why you take it, and your eGFR. Show it to every provider.
- Know your triggers. If you’re sick, dehydrated, or having surgery, your kidneys are under stress. Hold NSAIDs. Hold metformin. Call your nephrologist.
One patient on DaVita.com shared how her nephrologist used a KDIGO checklist to catch her metformin dose when her eGFR fell to 38. She avoided lactic acidosis. That’s the power of a system.
What’s Changing in 2025-2026
Guidelines aren’t static. The 2024 KDIGO update was a game-changer. But more is coming. The FDA plans to update its renal dosing guidance in 2026 using real-world data from electronic health records. That means drug labels will get smarter. Also, a standardized CKD medication safety checklist is due out in Q2 2026-designed for clinics and patients alike.Pharmacogenomics is also entering the picture. Researchers are studying how gene variations affect drug metabolism in CKD. In the next few years, we may see tests that tell you if you’re more likely to have bad reactions to certain drugs.
Meanwhile, hospitals are finally waking up. The Veterans Health Administration added eGFR alerts to their system in 2019. Result? A 37% drop in wrong doses. Other systems are catching on.
What to Do If You’re Already on a Risky Drug
If you’re taking something that’s not safe for your kidneys, don’t panic. Don’t quit cold turkey. Talk to your doctor. Here’s what to ask:- “Is this drug cleared by my kidneys?”
- “What’s the safe dose for my eGFR?”
- “Is there a safer alternative?”
- “Do I need blood tests to monitor this?”
For example, if you’re on a sulfonylurea, ask about GLP-1 agonists like semaglutide. They’re safer for kidneys and help with weight loss too. If you’re on NSAIDs for arthritis, ask about acetaminophen or physical therapy. Many CKD patients find relief without the risk.
And if you’re on a drug without clear dosing guidance for CKD-like some older antibiotics or antifungals-ask for a pharmacist consult. Clinical pharmacists specialize in this. They’re your secret weapon.
Final Thought: Knowledge Is Your Shield
Medication safety in kidney disease isn’t about fear. It’s about awareness. You don’t need to memorize every drug’s half-life. But you do need to know your eGFR. You need to know which pills to avoid. You need to speak up when something doesn’t feel right.CKD affects 37 million Americans. Thousands are hospitalized every year because a simple dose wasn’t adjusted. But with the right tools-like the KDIGO guidelines, one pharmacy, and a clear list of your meds-you can stay out of the hospital and keep your kidneys working longer.
Your kidneys can’t tell you what’s wrong. But you can learn to listen.
Can I still take ibuprofen if I have kidney disease?
No, it’s not safe. Ibuprofen and other NSAIDs reduce blood flow to the kidneys, which can cause acute kidney injury-especially if your eGFR is below 60. Even one or two doses can spike your creatinine. Use acetaminophen (Tylenol) instead for pain, and always check with your doctor before taking any OTC painkiller.
What if my eGFR changes suddenly?
If your eGFR drops quickly-like during an infection, dehydration, or after surgery-stop nephrotoxic drugs immediately. Hold metformin, NSAIDs, and certain antibiotics. Contact your nephrologist or primary care provider right away. Your medication doses need to be re-evaluated within 24-48 hours. Don’t wait for your next appointment.
Are SGLT2 inhibitors safe if I don’t have diabetes?
Yes. The 2024 KDIGO guidelines recommend SGLT2 inhibitors like dapagliflozin for people with CKD and albuminuria-even if they don’t have diabetes. These drugs slow kidney decline and reduce heart failure risk. Dosing stays the same regardless of kidney function, making them one of the few medications that don’t need adjustment in advanced CKD.
Why do some doctors still underdose ACE inhibitors?
Many doctors were trained to avoid ACE inhibitors if creatinine rises, thinking it meant kidney damage. But research shows that rise is actually a sign the drug is working to protect the kidneys. KDIGO 2024 calls this outdated thinking “suboptimal care.” Full doses reduce protein in the urine and slow disease progression-even when eGFR is below 30.
How often should I get my medications reviewed?
At least every 3 months if you have stage 3-5 CKD. More often if your eGFR is dropping, you’re hospitalized, or you start a new drug. A 2023 study found that patients who had quarterly medication reviews with their nephrologist had 50% fewer drug-related hospitalizations. Bring your full list of meds-including supplements and OTCs-to every appointment.

13 Comments
Vicky Zhang
15 January, 2026Oh my gosh, I just read this and I’m crying. My mom had CKD and she took ibuprofen for her arthritis because she didn’t know it was dangerous. One weekend she felt weird, went to the ER, and they said her kidneys were shutting down. We almost lost her. I wish someone had told us this sooner. Now I print out this whole article and tape it to the fridge. Every time she reaches for a pain pill, I say ‘remember the kidneys, mama.’ It’s annoying but it saves lives. Thank you for writing this.
I told my whole book club about it. We’re all going to start asking our doctors about eGFR. We’re not waiting for a crisis anymore.
Also, I started using one pharmacy. It was a pain switching, but now they flag everything. Last week they stopped me from picking up a cold med with pseudoephedrine. I didn’t even know it was in there. I felt like a superhero.
And yes, I carry my med list everywhere. Even to the grocery store. My pharmacist says I’m his favorite patient. I say I’m just smart.
People think kidney disease is silent, but it’s screaming. We just have to learn how to listen.
And SGLT2 inhibitors? My nephrologist put me on one last year. I don’t have diabetes. I thought he was crazy. Now I feel better than I have in years. No more swelling. No more fatigue. Just… normal. Thank you for telling the truth about this.
Don’t let fear stop you. Let knowledge guide you. Your kidneys are working hard. Give them a break.
And if you’re on NSAIDs? Stop. Just stop. Acetaminophen is fine. You don’t need to suffer. You just need to be smart.
I’m not a doctor. I’m a daughter. And I’m so glad I learned this before it was too late.
Susie Deer
16 January, 2026Doctors are useless. They dont know shit. I read this and I already know more than my nephrologist. I stopped all my meds cold turkey. Now Im fine. No more hospital visits. Simple.
Andrew Freeman
16 January, 2026bro i read this and i think its all just a big pharma scam
they want you to take expensive new drugs like finerenone so they can charge 10k a year
my abuela took aspirin for 40 years and shes 89 and still walks her dog
also eGFR is just a number they made up to sell more tests
if your pee looks clear and you dont feel like crap then why change anything
also i took ibuprofen last week and my creatinine went up but i felt better so who cares
they just want you scared so you buy their stuff
says haze
16 January, 2026What this article fails to articulate, and what most laypeople miss entirely, is the epistemological rupture between clinical guidelines and lived bodily experience. The KDIGO recommendations are not medical truths-they are statistical artifacts of population-level trials that erase heterogeneity. Your eGFR is not your kidney’s soul. It is a proxy, a reduction, a metric designed for billing codes and insurance reimbursement. The real damage occurs not from NSAIDs or metformin, but from the institutionalization of quantification as moral authority. You are not a number. You are not a creatinine curve. You are the organism that has survived 70 years of processed food, chronic stress, and systemic neglect-and now you are being told to surrender agency to a protocol written by a committee that has never held your hand during a dialysis session.
The real tragedy is not medication error-it is the commodification of vulnerability. SGLT2 inhibitors are not miracles. They are profit engines with a side effect of delayed progression. Finerenone? A patent extension dressed as innovation. The only thing that truly protects kidneys is dignity. And dignity doesn’t come from a checklist. It comes from being seen.
But I suppose if you’re going to live in a world where your worth is measured in mL/min/1.73m², then yes, by all means-carry your med list. Just remember: the algorithm doesn’t care if you’re lonely. Or afraid. Or tired. It just wants your numbers to be clean.
Alvin Bregman
18 January, 2026i like this post a lot
my uncle had kidney trouble and he used to take all kinds of pills from different doctors
we got him to use one pharmacy and it changed everything
they caught a drug combo that was making his potassium go crazy
he didn’t even know he was taking two things that did the same thing
now he’s doing better and he says he feels like he has his life back
also i started asking my doc about every new pill
even if it’s just for a cold
it feels weird at first but you get used to it
and yeah i carry my list
it’s in my wallet next to my id
no more guessing
just facts
simple
thank you for saying this
it matters
Sarah -Jane Vincent
19 January, 2026THIS IS A GOVERNMENT COVER-UP. NSAIDs are NOT dangerous. The FDA is in bed with Big Pharma to push expensive SGLT2 inhibitors that are linked to genital infections and amputations. They want you to think ibuprofen is poison so you’ll buy their patented $800/month drugs. The eGFR is manipulated. They use outdated formulas that make older people look worse than they are. I checked my own creatinine three times with a home kit-my numbers are fine. My doctor is scared to prescribe anything because he’s afraid of lawsuits. Meanwhile, people in other countries take NSAIDs daily and live to 90. This is fearmongering. And don’t get me started on finerenone-trials were funded by Bayer. They’re lying to you. Wake up. This isn’t medicine. It’s marketing.
Henry Sy
19 January, 2026my ex wife had stage 4 CKD and she was on every damn pill in the pharmacy
metformin, lisinopril, glipizide, ibuprofen, vitamin D, fish oil, turmeric, and some weird herbal tea from her cousin in Mexico
she had a seizure last year because her potassium hit 6.8
they had to shock her
she didn’t even know she was on a drug that was killing her
now she’s on SGLT2 inhibitors and she’s lost 40 pounds and she’s smiling again
but she still takes the herbal tea
she says it’s ‘natural’
idk man
the system is broken
but the meds? they work
if you’re on NSAIDs and you’re not dead yet
you’re just lucky
not smart
shiv singh
20 January, 2026in my country we dont have all these fancy drugs
we use garlic, lemon, and prayer
my father had CKD and he never took a single pill from a hospital
he drank warm water with lemon every morning
he lived to 84
you think your science is better?
your pills are poison
your labs are lies
you are trusting machines over wisdom
your kidneys will fail faster because you are afraid
not because of ibuprofen
because of your fear
and your arrogance
we dont need your guidelines
we need our ancestors
TooAfraid ToSay
21 January, 2026you know what’s really dangerous? trusting doctors who don’t even know how to pronounce ‘eGFR’
i saw a guy in the ER last month
he was on metformin with an eGFR of 22
the doctor said ‘oh you’re fine’
he almost died
and now he’s on dialysis
they don’t care
they’re just rushing through appointments
you have to be your own advocate
or you die
simple as that
and if you’re not screaming for your meds to be reviewed
you’re already dead
just walking
Robert Way
21 January, 2026hey i just wanted to say i read this and i think its amazing
i have a cousin with kidney disease and i told her about the one pharmacy thing
she was so mad at first because she had to switch
but now she says she feels safer
also i keep forgetting to write down my meds
so i started using my phone notes
and i take a picture every time i get a new prescription
its dumb but it helps
thanks for reminding me to be careful
also i think you spelled ‘glipizide’ wrong in the article
but i still loved it
Sarah Triphahn
22 January, 2026Let’s be honest: most people who read this won’t change a thing. They’ll scroll past, shrug, and keep taking their Advil. Why? Because awareness doesn’t equal action. Knowledge is not power-power is action. And action requires discomfort. Most people would rather die than admit they were wrong about a pill they’ve been taking for a decade. They’d rather risk kidney failure than face the inconvenience of switching to Tylenol. This isn’t about medicine. It’s about human denial. The real nephrotoxin isn’t ibuprofen-it’s complacency. And we’re all addicted.
Also, if you’re still on sulfonylureas? You’re not just at risk for hypoglycemia. You’re at risk for being the reason your family has to make funeral arrangements. You’re not just a patient. You’re a liability. And you’re not saving money by avoiding expensive drugs. You’re spending it on ER visits. That’s not frugal. That’s foolish.
Allison Deming
23 January, 2026It is imperative to recognize that the foundational premise of this article-that patient self-advocacy can supplant clinical expertise-is both dangerously naive and ethically precarious. While the KDIGO guidelines are indeed evidence-based, their application requires nuanced clinical judgment that cannot be reduced to a checklist. A patient who stops NSAIDs because they read a Reddit post may inadvertently precipitate hypertension or heart failure. A patient who discontinues metformin without monitoring may experience hyperglycemic crisis. The notion that carrying a medication list replaces the need for longitudinal care is not only misleading-it is a form of medical populism that erodes the very foundation of therapeutic trust.
Furthermore, the glorification of SGLT2 inhibitors as panaceas ignores the fact that they are contraindicated in volume-depleted patients, those with recurrent genital mycotic infections, and individuals with a history of DKA. Their use without proper patient selection and education is not innovation-it is negligence dressed in marketing.
True safety does not come from vigilance alone. It comes from collaboration. From the pharmacist who calls your doctor. From the nephrologist who remembers your name. From the nurse who checks your labs before you leave the clinic. To reduce this complex, life-sustaining system to a series of bullet points is to misunderstand the very nature of healing.
Do not mistake awareness for mastery. Do not confuse a checklist with competence. Your kidneys are not a spreadsheet. They are a miracle. And miracles require care-not just caution.
Andrew Freeman
23 January, 2026ok but what if your doctor is just lazy
my doc wont change my meds unless i bring him a printed copy of the kdigo guidelines
and then he says ‘hmm interesting’
and does nothing
so i had to go to a pharmacist
she looked at my list and said ‘you’re gonna die if you keep this’
she called my doctor and he changed it
so yeah
doctors are useless
pharmacists are the real heroes
and if you’re not talking to yours
you’re just waiting to die