Quercetin Medication Interaction Checker
Check Your Medications
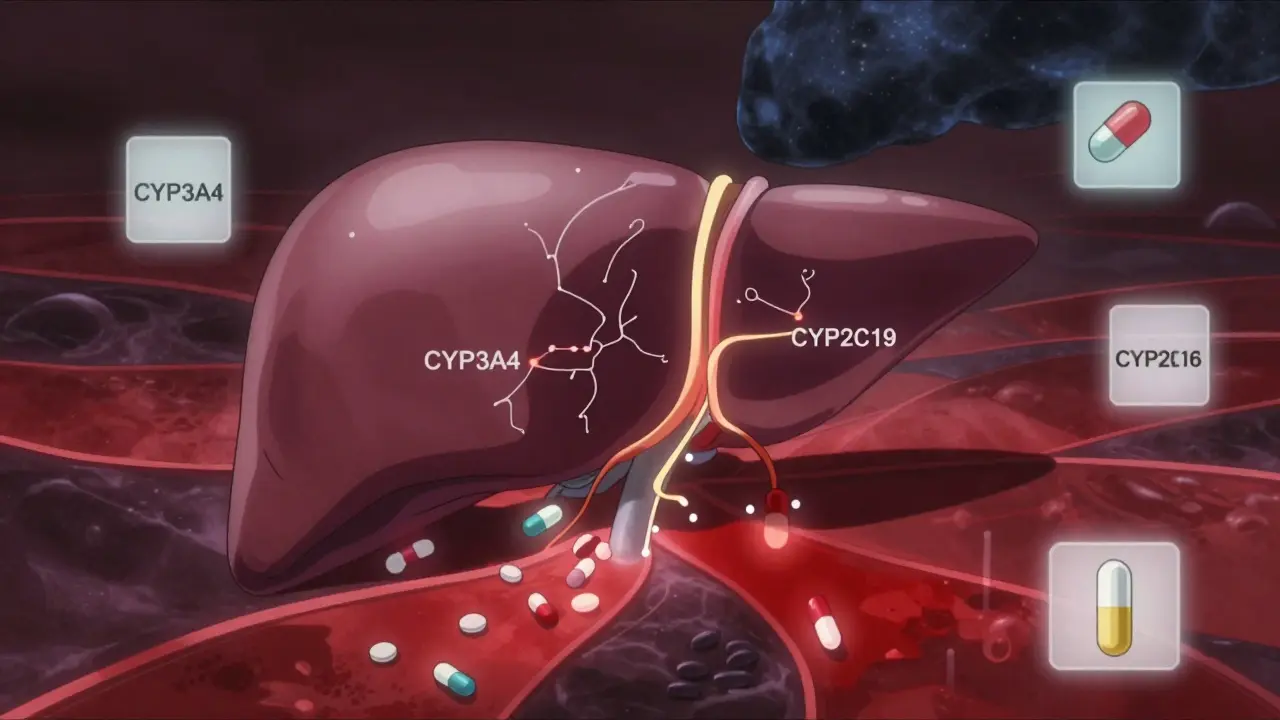
Enter your prescription medications to see if they interact with quercetin supplements. Results based on CYP3A4, CYP2D6, and CYP2C19 enzyme inhibition.
Many people take quercetin supplements thinking they’re just getting a natural boost from fruits and vegetables. But when you start popping high-dose pills-500 mg, 1,000 mg, even more-you’re not just eating an apple anymore. You’re introducing a powerful chemical that can change how your body handles prescription drugs. And that’s not something to ignore.
What Quercetin Actually Does to Your Liver
Quercetin is a flavonoid found in onions, apples, berries, and capers. In food, it’s harmless. But in supplement form, especially at doses above 500 mg daily, it acts like a brake on your liver’s drug-processing system. Specifically, it blocks enzymes called cytochrome P450, or CYP enzymes. These enzymes are responsible for breaking down about 75% of all prescription medications. The big ones affected are CYP3A4, CYP2D6, and CYP2C19. These aren’t obscure enzymes-they handle common drugs like statins, blood thinners, antidepressants, and even some cancer treatments. When quercetin shuts them down, your body can’t clear those drugs as fast. That means more of the drug stays in your bloodstream. For some medications, that’s dangerous. A 2020 study in Nutrients showed that at concentrations you’d reach with a 1,000 mg supplement, quercetin blocked up to 85% of CYP2D6 activity. That’s stronger than some prescription inhibitors. It also cut CYP3A4 activity by 40-60%. That’s not a small effect. It’s the kind of change that can turn a safe dose into a toxic one.Which Medications Are at Risk?
If you’re taking any of these, quercetin supplements could be a problem:- Warfarin - Quercetin can raise your INR by 0.8 to 1.5 points. That’s enough to increase bleeding risk significantly.
- Cyclosporine - Used after organ transplants. Quercetin can push levels up by 30-50%, raising the chance of kidney damage.
- Abemaciclib - A breast cancer drug. Quercetin increases its blood levels by 25-35%, which can worsen side effects like diarrhea and low white blood cell counts.
- Acenocoumarol - Another blood thinner. Similar risks to warfarin.
- Apixaban and Rivaroxaban - These direct oral anticoagulants (DOACs) are especially risky. Quercetin doesn’t just affect liver enzymes-it also blocks transporters that move these drugs out of your gut and kidneys. That means more drug gets absorbed and stays in your system longer.
- Statins - Like simvastatin and atorvastatin. Higher levels mean more muscle pain, and in rare cases, life-threatening rhabdomyolysis.
- Antidepressants - Such as fluoxetine and sertraline, metabolized by CYP2D6. Quercetin can push levels into the toxic range, causing serotonin syndrome.
Why Food Is Safe, But Supplements Aren’t
You might be thinking: “I eat onions every day. Why is that okay?” Because the amount of quercetin in food is tiny. One medium onion has about 20-40 mg. Even a cup of apples or berries gives you less than 10 mg. Your body absorbs only a fraction of that. Plus, in food, quercetin is bound to sugar molecules (glycosides), which slow absorption and reduce its enzyme-blocking power. Supplements change everything. They deliver pure, unbound quercetin-often 500 mg or more per capsule. That’s 10 to 50 times what you’d get from food. And it’s absorbed faster and more completely. That’s why the European Food Safety Authority (EFSA) says supplements over 1,000 mg/day raise real concerns.
Who’s Most at Risk?
It’s not just about the dose. Some people are more vulnerable:- People over 65 - Their liver and kidney function slows down. Quercetin and its metabolites stick around longer, increasing interaction risk by 25-40%.
- People on multiple medications - If you’re taking five or more drugs, the chance that one of them is affected by quercetin goes up fast. This is called polypharmacy, and it’s common in older adults.
- People with liver disease - Their CYP enzymes are already impaired. Adding quercetin pushes them over the edge.
- People taking drugs with narrow therapeutic windows - These are medications where the difference between a good dose and a dangerous one is small. Warfarin, cyclosporine, and some seizure meds fall into this category.
What the Experts Say
Dr. Basheer Kerem from Hebrew University showed in animal studies that quercetin can double the amount of certain drugs in the blood. That’s not theoretical-it’s measurable. The FDA calls quercetin a “dietary supplement of concern” and says drug makers should test for interactions with it. The American Society of Health-System Pharmacists (ASHP) doesn’t mince words: avoid quercetin entirely if you’re on DOACs. The University of California San Francisco has a clear protocol: if you’re on CYP3A4, CYP2D6, or CYP2C19 substrates, don’t take more than 500 mg of quercetin per day. And if you’re elderly or on multiple meds? Don’t take it at all.
What You Can Do
If you’re already taking quercetin supplements:- Check your meds. Look up each prescription on a drug interaction checker (like Medscape or Micromedex). If it’s metabolized by CYP3A4, CYP2D6, or CYP2C19, be cautious.
- Don’t assume “natural” means safe. Quercetin is natural, but so is poison ivy. Natural doesn’t mean harmless.
- Talk to your pharmacist. They see drug interactions every day. Bring your supplement bottle to your next visit.
- If you must take it, separate it from your meds. Take quercetin at least 4-6 hours before or after your prescription. That can cut interaction risk by 30-50%.
- Stop if you feel unusual symptoms. Unexplained bruising, muscle pain, dizziness, or nausea could be signs of a drug interaction.
The Bigger Picture
The global quercetin supplement market hit $387 million in 2022. Nearly 18 million Americans take it. Over 40% of them take more than 500 mg daily. That’s a lot of people unknowingly risking drug interactions. And here’s the problem: supplements aren’t regulated like drugs. Manufacturers don’t have to prove safety or test for interactions before selling. The FDA has issued 17 warning letters to quercetin brands for making false claims-but they can’t pull them off the shelf. The good news? The FDA is working on new labeling rules for high-risk supplements like quercetin, expected in 2024. Until then, the responsibility falls on you.Bottom Line
Quercetin from food? Fine. Quercetin from a bottle? Proceed with extreme caution. If you’re on any prescription medication, especially blood thinners, cancer drugs, or heart medications, high-dose quercetin isn’t worth the risk. Talk to your doctor or pharmacist before taking it. Your meds might be fine. But your liver doesn’t know the difference between an apple and a pill. And it won’t warn you until it’s too late.Can I take quercetin if I’m on blood pressure medication?
It depends. If your blood pressure medication is metabolized by CYP3A4 (like amlodipine, diltiazem, or verapamil), quercetin can raise its levels and cause low blood pressure, dizziness, or fainting. If you’re on a beta-blocker like metoprolol (CYP2D6), the same risk applies. Don’t assume it’s safe just because it’s a common drug. Check with your pharmacist or doctor before combining them.
Is quercetin safe with over-the-counter painkillers like Tylenol?
Acetaminophen (Tylenol) is mostly processed by a different enzyme, UGT, but quercetin can still increase its levels by 20-30% by interfering with liver transporters. That’s usually not dangerous at standard doses, but if you’re taking high doses of Tylenol regularly or have liver issues, it could raise your risk of liver damage. It’s safer to avoid high-dose quercetin if you’re using Tylenol daily.
Does quercetin interact with vitamin D or calcium supplements?
No. Vitamin D and calcium aren’t metabolized by CYP enzymes or transported by the same pathways affected by quercetin. You can safely take them together. But if your calcium supplement contains other ingredients-like magnesium or zinc-check those too. Some minerals can interfere with absorption, but not through the same mechanism as quercetin.
How long does quercetin stay in my system?
Quercetin has a short half-life-about 3-4 hours-but its metabolites linger much longer, sometimes up to 24 hours. That means even if you take it in the morning, it can still affect how your body processes a medication you take at night. This is why spacing doses by 4-6 hours helps, but doesn’t fully eliminate risk.
Are there safer alternatives to quercetin for inflammation?
Yes. Curcumin (from turmeric) has strong anti-inflammatory effects and doesn’t significantly inhibit CYP enzymes at normal doses. Omega-3 fatty acids from fish oil also reduce inflammation without drug interaction risks. Ginger and boswellia are other options with better safety profiles. Always check, but these are generally safer than high-dose quercetin.
Can I take quercetin if I’m not on any medications?
If you’re not taking any prescription or over-the-counter drugs, and you don’t have liver or kidney disease, occasional use of quercetin supplements is likely low-risk. But there’s still no proven benefit for healthy people. Most claims about immune boosting or allergy relief aren’t backed by strong human trials. If you’re healthy, focus on eating more onions, apples, and berries instead.

14 Comments
Sally Denham-Vaughan
3 January, 2026Okay but like… I’ve been taking 1000mg of quercetin for my allergies and I’m on lisinopril. Should I be sweating? I didn’t think a fruit thing could mess with my BP med. 😅
Bill Medley
3 January, 2026Quercetin inhibits CYP3A4 and CYP2D6. This is well-documented. The risk is real and clinically significant.
Richard Thomas
4 January, 2026It’s strange, isn’t it? We’ve been conditioned to think ‘natural’ equals ‘safe’-as if the forest doesn’t contain poison ivy, hemlock, and deadly nightshade. Quercetin isn’t the villain; it’s just chemistry. And chemistry doesn’t care if you bought it at Whole Foods or a pharmacy. The liver doesn’t know the difference between an apple and a capsule. It just sees molecules. And when those molecules block enzymes that have spent decades evolving to keep us alive, things get… complicated. We want magic pills that fix everything without consequence, but biology doesn’t work that way. It’s not a bug-it’s a feature of evolution. We’re just now catching up to what plants have been doing for millennia.
Andy Heinlein
6 January, 2026YOOO I just took quercetin this morning and I’m on atorvastatin 😳 I’m gonna stop right now. Also why is everyone so chill about this?? Like we’re all just popping pills like candy and hoping for the best?? 🙃
Todd Nickel
7 January, 2026There’s a significant pharmacokinetic interaction between quercetin and CYP3A4 substrates, particularly those with narrow therapeutic indices such as cyclosporine and apixaban. The inhibition constant (Ki) for quercetin against CYP3A4 is approximately 2.7 µM, which is easily exceeded with standard supplement dosing (500–1000 mg). Furthermore, quercetin’s metabolites-particularly quercetin glucuronides-retain inhibitory activity and have prolonged half-lives, meaning even spaced dosing doesn’t fully mitigate risk. The FDA’s recognition of quercetin as a dietary supplement of concern is understated; the lack of mandatory interaction labeling is a regulatory failure. The burden of safety should rest with manufacturers, not patients.
gerard najera
8 January, 2026Natural doesn’t mean safe.
Stephen Gikuma
9 January, 2026Big Pharma doesn’t want you to know this. They sell statins, they sell blood thinners, and now they’re trying to scare you off a $10 supplement so you keep buying their $500/month pills. This is all about profit. Quercetin’s been used for centuries. They just don’t patent nature.
Bobby Collins
11 January, 2026They’re lying about the ‘natural’ thing… I saw a video on TikTok that said the FDA banned quercetin in 2021 but they just renamed it ‘bioflavonoid complex’ and kept selling it. They’re hiding it from us. I don’t trust anyone anymore 😔
Layla Anna
12 January, 2026OMG I’m so glad I found this post!! I’ve been taking quercetin with my antidepressant and I’ve been feeling weirdly zoned out lately… I’m gonna stop and talk to my pharmacist tomorrow 💛
Heather Josey
14 January, 2026This is an exceptionally well-researched and clinically relevant summary. The distinction between dietary intake and pharmacological dosing is critical, and the emphasis on pharmacist consultation cannot be overstated. Public health education on supplement-drug interactions remains grossly inadequate. I urge all healthcare providers to routinely screen for supplement use during medication reconciliation.
Donna Peplinskie
14 January, 2026Thank you so much for this-really, thank you. I’m a nurse in Toronto and I’ve seen two patients with rhabdomyolysis after starting quercetin while on simvastatin. One was 72, the other was 58. Neither knew it could do this. I wish every supplement bottle had a warning label like this. I’ve been printing out copies to hand out at my clinic.
Olukayode Oguntulu
15 January, 2026Let’s be clear: the CYP450 system is not some mystical biochemical oracle-it’s a metabolic bottleneck engineered by evolution to handle xenobiotics. Quercetin, as a polyphenolic flavonoid, acts as a competitive inhibitor at the heme iron center of CYP3A4, effectively downregulating phase I metabolism. This is not ‘natural’-it’s pharmacological interference masquerading as wellness. The real tragedy is not quercetin, but the neoliberal commodification of biochemistry into ‘supplements’ devoid of pharmacovigilance. We’ve outsourced our biological literacy to Amazon reviews.
Matthew Hekmatniaz
16 January, 2026There’s something poetic about how we treat food as sacred and pills as dangerous-yet we eat onions daily and pop quercetin capsules like candy. Maybe it’s not the quercetin that’s the problem. Maybe it’s the idea that we can isolate one compound from nature and expect it to behave like a drug without consequences. We’ve forgotten that plants don’t exist to heal us-they exist to survive. And sometimes, their survival strategy is to mess with our enzymes.
Liam George
18 January, 2026They’re hiding the truth. The FDA’s ‘warning letters’? Just PR theater. The real danger? The fact that quercetin is being used in military research to enhance drug retention in soldiers. They don’t want you to know that what you’re taking is the same tech they’re using to make soldiers’ meds last longer. You’re not a consumer-you’re a test subject.