Statins Cognitive Risk Calculator
How Statins May Affect Your Memory
This tool helps you understand potential cognitive side effects based on your statin type. Remember: Most people experience no memory issues. When symptoms occur, they're often temporary and reversible.
Your Statin Type
Lipophilic Statins
(Atorvastatin, Simvastatin, Lovastatin, Fluvastatin, Pitavastatin)
These cross the blood-brain barrier more easily. Studies show 1.42x higher likelihood of memory complaints.
Hydrophilic Statins
(Pravastatin, Rosuvastatin)
These stay mostly in the liver. Fewer cognitive side effects reported.
Is This About You?
Results
Disclaimer: This tool is informational only. Please consult your doctor for medical advice.
Memory Concerns? Here's What the Science Says
Research shows: 28% of statin users report memory problems, but only 8% show actual decline on cognitive tests.
This gap suggests the nocebo effect plays a role - when you expect side effects, your brain may start noticing ordinary memory lapses as problems.
Great News: You're Likely Fine
Most people on statins experience no memory issues. The article mentions that 39 million Americans take statins with no cognitive problems.
What Should You Do?
Track it: Keep a journal of when symptoms occur and what else was happening (sleep, stress, diet).
Don't assume it's the statin: Memory issues can come from many sources - sleep apnea, vitamin deficiencies, depression, or stress.
Consult your doctor: Discuss whether switching to a hydrophilic statin (pravastatin or rosuvastatin) might help.
When you start taking a statin to lower your cholesterol, you’re doing it to protect your heart. But then, out of nowhere, you forget where you put your keys. Or you walk into a room and can’t remember why. Or you struggle to find the right word mid-sentence. If that’s happened to you, you’re not alone. And you’re not imagining it. But here’s the thing: statins might not be the real culprit.
What Are Statins, Really?
Statins are a class of drugs designed to lower LDL (bad) cholesterol. They work by blocking an enzyme in your liver called HMG-CoA reductase, which your body uses to make cholesterol. Less cholesterol production means less plaque buildup in your arteries, which lowers your risk of heart attack and stroke.
There are seven statins approved for use in the U.S.: atorvastatin (Lipitor), simvastatin (Zocor), pravastatin (Pravachol), rosuvastatin (Crestor), lovastatin (Mevacor), fluvastatin (Lescol), and pitavastatin (Livalo). Millions of Americans take them - nearly 39 million in 2023 alone. For most people, they’re safe and life-saving.
But in the early 2000s, doctors started hearing from patients: "I’m forgetting things since I started this pill." The FDA took notice. In 2012, they updated statin labels to include memory loss and confusion as possible side effects. That’s when the panic started.
Do Statins Actually Cause Memory Loss?
The short answer: sometimes - but rarely, and usually not permanently.
Here’s what the science says. A 2015 study in JAMA Internal Medicine found a 3.78-times higher risk of acute memory loss within 30 days of starting a statin. Sounds scary, right? But here’s the twist: the same risk appeared with other cholesterol-lowering drugs that aren’t statins. That suggests it’s not the statin itself - it’s the fact that people are now paying closer attention to their memory after starting a new medication. This is called detection bias.
More telling? Objective testing. In study after study, when researchers used brain tests - memory recall, attention span, processing speed - they found almost no difference between people on statins and those on placebo. One 2020 study in the Journal of General Internal Medicine found that 28% of statin users reported memory problems. But only 8% showed actual decline on cognitive tests.
That gap between what people feel and what tests show points to the nocebo effect - the opposite of placebo. If you believe a drug might cause brain fog, your brain starts looking for it. Suddenly, forgetting your password feels like a sign of dementia. It’s not. It’s stress, sleep, aging, or anxiety.
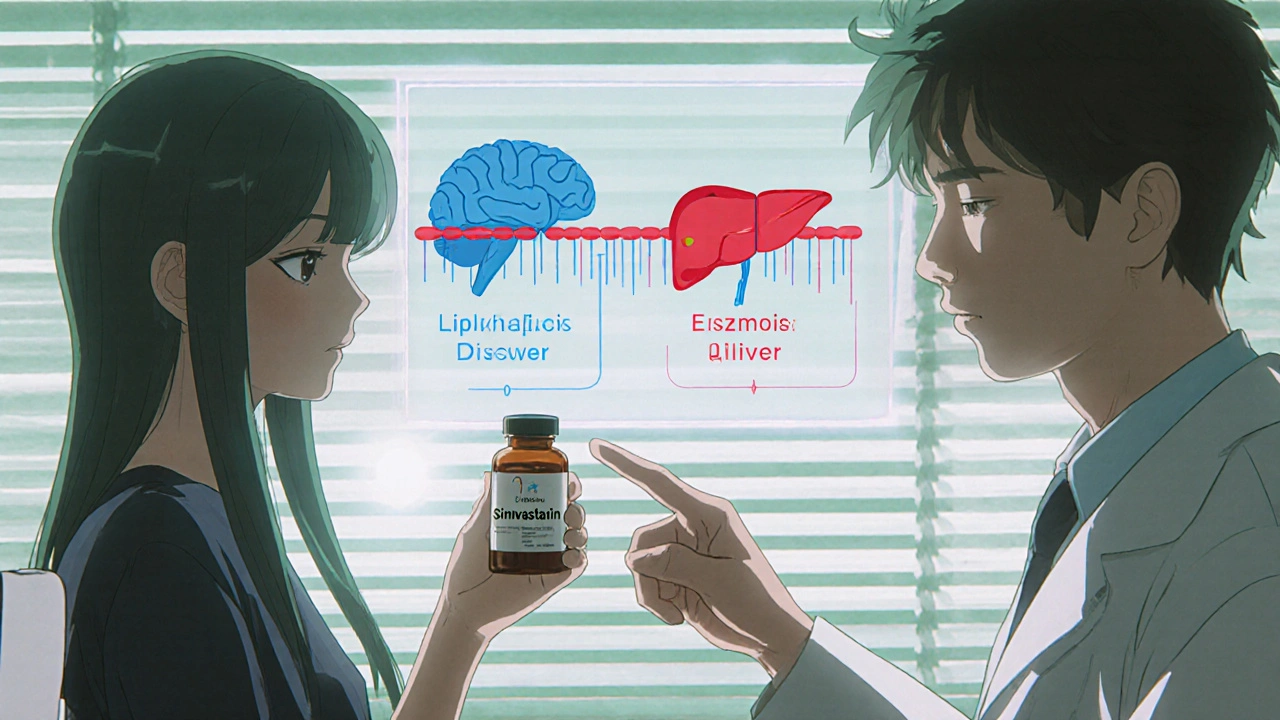
Lipophilic vs. Hydrophilic: The Blood-Brain Barrier Factor
Not all statins are created equal. Some cross into the brain more easily than others.
Statins fall into two groups based on how well they dissolve in fat:
- Lipophilic statins (atorvastatin, simvastatin, lovastatin, fluvastatin, pitavastatin) can cross the blood-brain barrier. That means they enter brain tissue.
- Hydrophilic statins (pravastatin, rosuvastatin) can’t. They stay mostly in the liver.
Studies show lipophilic statins are linked to more self-reported memory complaints. A 2023 analysis of 48,732 patients found they were 1.42 times more likely to be reported as causing cognitive issues. But again - objective tests didn’t show a difference.
That’s why doctors often suggest switching to pravastatin or rosuvastatin if memory problems show up. Many patients report feeling better within weeks. Not because the drug was "bad," but because the brain stopped getting exposed to something it was sensitive to.
Real Stories, Real Reversals
Let’s talk about real people.
In a 2003 study, Dr. Beatrice Golomb reviewed 60 case reports. Half of the patients noticed memory issues within 60 days of starting a statin. When they stopped taking it, 56% got better. Four of them took the same statin again - and the memory problems came back.
Reddit’s r/Statins community analyzed over 1,200 posts in 2023. Of those who reported brain fog:
- 68% said symptoms started within 3 months
- 74% felt better within 4 weeks of stopping
These aren’t rare. They’re real. But they’re also temporary. And reversible.
One woman in her late 60s, on simvastatin for five years, started forgetting names of close friends. She stopped the drug on her own. Within three weeks, her memory returned. She switched to rosuvastatin. No more issues. She’s still on it, five years later.
That’s not a side effect. That’s a signal.
Statins Might Actually Protect Your Brain
Here’s the twist most people don’t know: statins might lower your risk of dementia.
A 2022 analysis from the Alzheimer’s Society looked at 36 studies with over 1.2 million people. Those on statins had a 21% lower risk of developing dementia overall. For vascular dementia - caused by poor blood flow to the brain - the risk dropped by 33%.
Why? Because statins don’t just protect your heart. They protect your brain’s blood vessels. Strokes and mini-strokes are major causes of cognitive decline. By reducing cholesterol and inflammation, statins help keep those vessels clear.
The Rotterdam Study, which followed 12,567 people for 15 years, found statin users had 27% fewer cases of dementia. That’s not a fluke. That’s a pattern.
So here’s the paradox: a drug that might cause short-term memory glitches in a small number of people could be preventing long-term brain damage in millions.
What Should You Do If You’re Worried?
If you’re on a statin and notice memory lapses, don’t panic. Don’t quit cold turkey. Do this instead:
- Track it. Keep a simple journal: When did it start? What happened? Was it worse on certain days? Did you sleep poorly? Were you stressed?
- Don’t assume it’s the statin. Other things cause memory issues: sleep apnea, vitamin B12 deficiency, thyroid problems, depression, even dehydration.
- Talk to your doctor. Ask: "Could this be the statin?" Then ask: "Can we try switching to pravastatin or rosuvastatin?"
- Try a "statin holiday." Your doctor might suggest stopping the drug for 4-6 weeks. If your memory improves, then restarting it confirms the link. If not, the statin isn’t the issue.
Most doctors won’t stop a statin unless symptoms are severe and clearly tied to the drug. Why? Because the risk of heart attack or stroke is far greater than the risk of temporary memory issues.
When to Keep Taking Statins - Even If You’re Worried
If you’ve had a heart attack, stroke, or have diabetes, high blood pressure, or a family history of early heart disease - statins are likely saving your life.
Dr. JoAnn Manson from Harvard says it plainly: "The benefits clearly outweigh the risks for people who need them."
The American Heart Association and American College of Cardiology agree. Their 2018 guidelines say: don’t stop statins because of vague memory complaints. Look for other causes first.
And here’s the bottom line: if you’ve been on a statin for years and feel fine? Don’t stop. You’re not at risk.
If you started one last month and feel foggy? Talk to your doctor. Switch if needed. But don’t assume the worst.
The Bigger Picture
Statins are one of the most studied drugs in medical history. We know how they work. We know who benefits. We know who doesn’t.
Memory loss isn’t a common side effect. It’s a rare one. And when it happens, it’s usually temporary. The science doesn’t support the fear. But it does support caution - and communication.
Your brain is important. Your heart is too. You don’t have to choose one over the other. You just need to work with your doctor to find the right balance.
Most people on statins never have a problem. For those who do, the fix is simple: switch the drug, give it time, and look for other causes. Your memory will likely come back. And your heart will stay protected.


12 Comments
Allison Turner
28 November, 2025This is just another case of people blaming their meds for being lazy. I forget where I put my keys every day. It's called aging, not statins.
Emma louise
28 November, 2025Oh wow, so now Big Pharma is telling us our brains are lying to us? Next they'll say the sun doesn't rise. I stopped my statin after my brain turned to mush. No regrets.
Gaurav Sharma
28 November, 2025Scientifically, the nocebo effect is well-documented. However, the emotional weight of cognitive decline is not to be dismissed. One must balance evidence with empathy.
Rhiana Grob
29 November, 2025It's important to remember that while statins are statistically safe for most, individual experiences matter. I've seen patients regain clarity after switching to rosuvastatin. It's not about fear-it's about listening.
Darrel Smith
30 November, 2025Let me tell you something. I was on Lipitor for 7 years. Started forgetting my daughter's birthday. Thought I was getting Alzheimer's. Went to my doctor, he said 'it's probably the statin.' I switched to pravastatin. Three weeks later, I remembered her name. I cried. Don't tell me this isn't real. This isn't science fiction-it's my life.
archana das
2 December, 2025In India, we have many elderly people on statins. Most don't report memory issues. Maybe it's diet, maybe it's stress, maybe it's how we talk about medicine. We don't panic. We observe. And we trust our doctors.
Emma Dovener
2 December, 2025One of my patients, 72, had a mild TIA last year. Started on atorvastatin. Within weeks, she couldn't recall her grandchildren's names. We switched to rosuvastatin. Within 21 days, her memory returned. She now calls me her 'memory saver.' This isn't anecdotal-it's clinical.
Melania Rubio Moreno
3 December, 2025statins r bad fr my brain. i stopped em. now i eat garlic and yoga. my mind is clear. the docs dont wanna hear it but i know what i felt.
steve stofelano, jr.
4 December, 2025While the aggregate data demonstrates a negligible cognitive impact from statin use, the phenomenological experience of cognitive disturbance remains a valid clinical concern. It is imperative that clinicians acknowledge patient-reported outcomes as complementary to objective neuropsychological assessment.
Shubham Semwal
4 December, 2025You think you're special because you forgot your keys? Everyone forgets things. Statins are saving millions from heart attacks. Stop whining and take your pill. Your brain's fine.
Sam HardcastleJIV
6 December, 2025It is curious how the modern medical paradigm so readily dismisses subjective experience as mere nocebo. Yet, when a patient reports a change in cognition following pharmacological intervention, we are expected to accept statistical averages over personal truth. This is not science-it is epistemological arrogance.
sharicka holloway
8 December, 2025I used to be the person who told everyone to just take their statins. Then my mom started spacing out, forgetting her own meds. We switched her to pravastatin. Within a month, she was back to telling me how to raise my kids. Don’t ignore the signs. Talk to your doctor. No shame in switching.