When bone loss goes beyond prevention
Most people hear about osteoporosis as something you prevent-take calcium, get vitamin D, do weight-bearing exercise. But for those with severe bone loss, prevention isn’t enough. When your T-score drops below -2.5 and you’ve already broken a bone-or are at high risk of it-your body needs more than just slowing down the decay. It needs to rebuild.
That’s where anabolic agents like teriparatide and abaloparatide come in. These aren’t your average osteoporosis pills. They’re injectable drugs designed to actually grow new bone, not just stop it from breaking down. Think of them as construction crews for your skeleton, not just security guards.
Both drugs are FDA-approved for postmenopausal women and men with high fracture risk. Both are given as daily shots under the skin. Both have been shown to cut fracture risk by more than half in some cases. But they’re not the same. And the difference matters-especially if you’ve had a hip fracture, care about side effects, or are paying out of pocket.
How teriparatide and abaloparatide work (and why it matters)
Teriparatide is a piece of the natural parathyroid hormone-specifically, the first 34 amino acids. It’s been around since 2002 and was the first drug of its kind. Abaloparatide came later, in 2017, and it’s a synthetic copy of a different hormone: PTHrP. That might sound like chemistry jargon, but here’s the real-world impact.
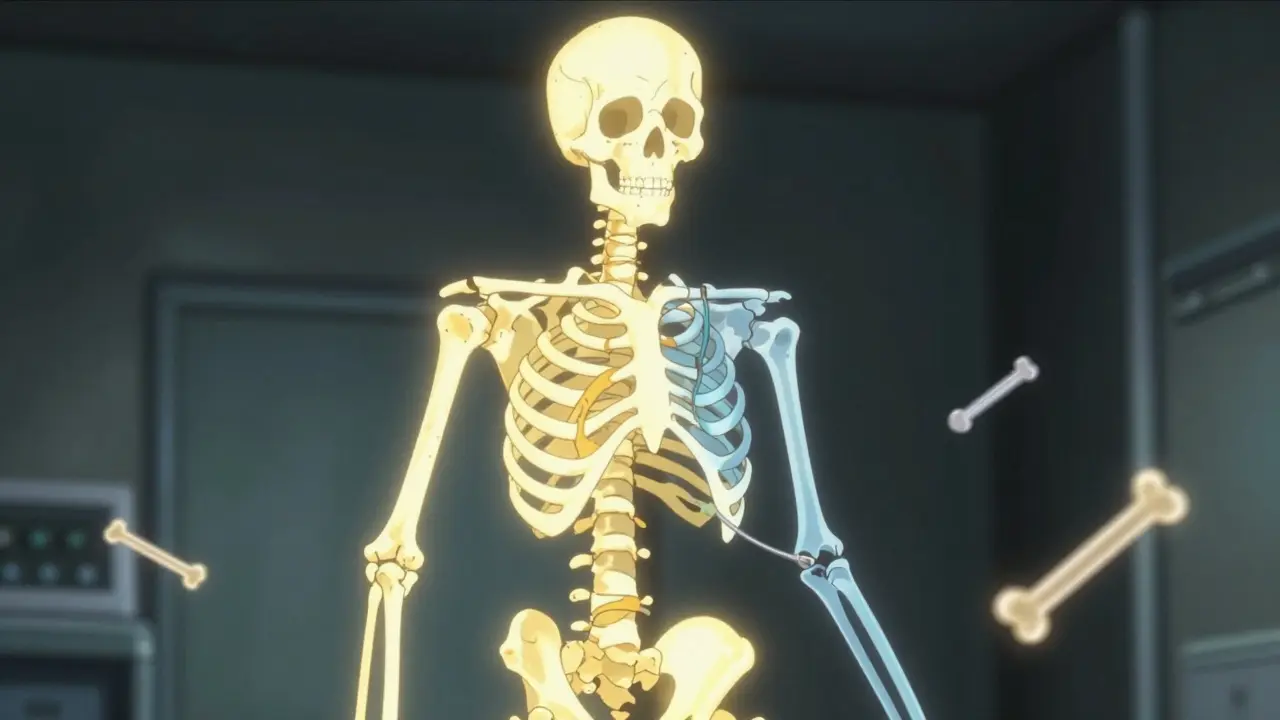
Teriparatide binds to the same receptor on bone cells in two ways: one that builds bone and one that breaks it down. It’s like a switch that turns on both the hammer and the chisel. Abaloparatide? It’s more selective. It mostly activates the bone-building side and barely touches the breaking-down side. That’s why studies show it causes less high calcium in the blood-hypercalcemia-than teriparatide.
In the ACTIVE trial, 3.4% of people on abaloparatide had high calcium levels. On teriparatide? 6.4%. That’s nearly double. For someone with kidney issues or a history of kidney stones, that difference isn’t just a number-it’s a reason to choose one drug over the other.
Which one builds bone better?
The numbers don’t lie. In the same ACTIVE trial, after 18 months:
- Abaloparatide increased total hip bone density by 3.41%
- Teriparatide? Just 2.04%
That’s a 1.37% difference. Sounds small? In bone terms, it’s huge. Hip bone density is the best predictor of hip fracture risk. If you’re over 70, have a T-score below -3.0, and your hip is your biggest worry, abaloparatide gives you a measurable edge.
Lumbar spine gains were similar at 18 months, but abaloparatide showed faster gains early on-6.58% at 6 months versus 5.25% for teriparatide. That’s important if you’re trying to get results before surgery, or if you’re worried about falling in the next few months.
And here’s something practical: in a 2024 real-world study of over 43,000 women, those on abaloparatide had 17% fewer hip fractures than those on teriparatide. That’s not just a lab finding-it’s a life-saving difference.
Fracture reduction: It’s not just about the spine
Many osteoporosis drugs work well on spinal fractures. That’s because the spine is made of spongy bone, which responds quickly to stimulation. But the hip? That’s dense, cortical bone. Harder to rebuild.
Abaloparatide doesn’t just do better on the hip-it does significantly better. The ACTIVE trial showed a 86% reduction in new vertebral fractures with abaloparatide compared to placebo. Teriparatide? About 65%. But the real win for abaloparatide was in nonvertebral fractures-especially hip fractures.
In the real world, people on abaloparatide had 12% fewer nonvertebral fractures than those on teriparatide. That’s not just statistical noise. That’s someone avoiding a broken hip, a hospital stay, a year of rehab, or worse.
Side effects: More than just dizziness
Both drugs can cause dizziness, nausea, and leg cramps. About 40% of people on teriparatide report dizziness. On abaloparatide? Closer to 30%. That’s a noticeable difference for someone trying to get through the day without feeling off-balance.
Injection site reactions? More common with teriparatide-68% of users report redness or itching at the injection spot. For abaloparatide, it’s 52%. That’s a 23% drop. Not huge, but meaningful if you’re injecting yourself every day for 18 months.
The biggest concern? Hypercalcemia. As mentioned, it’s twice as common with teriparatide. That’s not just a lab result. High calcium can cause fatigue, confusion, kidney stones, and even heart rhythm problems. For older patients, especially those on diuretics or with mild kidney disease, this can be dangerous.
Patient forums show people switching from teriparatide to abaloparatide specifically because their calcium levels stayed too high. One Reddit user wrote: “Switched after persistent hypercalcemia; calcium levels normalized within 3 months while maintaining BMD gains.” That’s not anecdotal fluff-it’s a pattern.
Cost and access: The hidden deciding factor
Let’s be honest: if one drug works just as well and costs half as much, most people will pick the cheaper one.
Teriparatide became generic in January 2024. The price dropped nearly 40%. Now it’s around $4,200 a month. Abaloparatide? Still brand name. Around $5,750. That’s $1,500 more per month. $18,000 more per year.
Insurance coverage? 44% of abaloparatide users report prior authorization denials or step therapy requirements. For teriparatide? Only 28%. Many insurers still require you to try teriparatide first-even if abaloparatide is a better fit.
A 2023 analysis found that 32% of people stopped teriparatide within a year. For abaloparatide? Only 24%. Why? Side effects, yes-but also cost. People just can’t afford it.
Who gets which drug? Real-world guidelines
The American Association of Clinical Endocrinologists (AACE) gives clear guidance:
- If your hip T-score is -3.0 or lower → abaloparatide is preferred
- If your spine is the main issue and cost is a barrier → teriparatide is still first-line
- If you’ve had a prior hip fracture → abaloparatide has stronger evidence
- If you have kidney disease or a history of high calcium → avoid teriparatide
Dr. Benjamin Leder, lead researcher of the ACTIVE trial, puts it simply: “Abaloparatide’s selective action gives you more bone growth with less bone breakdown. That’s the goal.”
But Dr. Ethel Siris, a respected osteoporosis expert, reminds us: “The absolute benefit difference is small. Is $18,000 a year worth a 0.3% lower fracture risk? For some, yes. For others, no.”
There’s no one-size-fits-all. It’s about your bones, your body, your wallet.

What happens after 18 months?
Neither drug is meant to be taken forever. The FDA limits use to 18-24 months because long-term safety data is limited. After that, you switch to an antiresorptive drug-usually alendronate (Fosamax) or denosumab (Prolia).
The ACTIVE-EXTEND trial showed something powerful: if you take abaloparatide for 18 months, then switch to alendronate, you keep 68% of your hip bone gains at 3.5 years. For teriparatide followed by alendronate? Around 60%.
That’s not a huge gap-but it’s enough to matter if you’re trying to avoid a second fracture. The key is timing. Don’t stop the injection and do nothing. The moment you stop, bone loss resumes. The transition has to be planned.
What’s next? Weekly shots and longer use
The biggest problem with both drugs? Daily injections. People forget. They get tired. They panic about needles. That’s why Radius Health is testing a weekly version of abaloparatide. Phase 3 trials ended in late 2023. Results are due mid-2025.
If it works, adherence could jump from 70% to over 90%. That’s huge.
The FDA is also pushing for studies on longer-term use. Right now, we don’t know what happens if you take these drugs for 3 or 4 years. Some doctors are already doing it off-label-but without data, it’s risky.
Bottom line: Choose based on your risk, not just your doctor’s habit
Teriparatide is the old workhorse. Proven. Cheaper. Available as a generic. But it comes with more side effects and less hip protection.
Abaloparatide is the newer, smarter option. Better for hips. Fewer high calcium episodes. Lower discontinuation rates. But it’s expensive and harder to get covered.
If you’re over 70, have a hip T-score under -3.0, or have had a nonvertebral fracture, abaloparatide gives you a real advantage.
If cost is tight, your kidneys are iffy, or your spine is your main concern-teriparatide still does the job.
Talk to your doctor. Ask for your T-scores. Ask about your fracture risk. Ask about insurance. Don’t just accept the first option they give you.
Your bones don’t care about brand names. They care about what works for you-and what you can stick with.


9 Comments
Paul Mason
6 January, 2026I've been on teriparatide for 14 months and my calcium levels went through the roof. Switched to abaloparatide last month and my doc says my numbers are finally stable. No more dizziness either. Seriously, if you got kidney issues, don't sleep on this.
Christine Joy Chicano
7 January, 2026The 1.37% difference in hip bone density isn't small-it's clinically significant. When you're over 70 and your hip is the weak link, that's not statistics, that's mobility. Abaloparatide's selectivity for the PTH1R receptor means less catabolic noise. It's like upgrading from a sledgehammer to a scalpel.
steve rumsford
8 January, 2026I got the abaloparatide pen and honestly? It’s less painful than I expected. The needle’s tiny. Still hate the daily thing though. Wish they’d just make it weekly already.
Anastasia Novak
9 January, 2026So let me get this straight-$18k a year for a drug that gives you a 0.3% edge? That’s not medicine, that’s corporate exploitation. Pharma’s just milking the fear of hip fractures. Teriparatide’s fine. Stop falling for the marketing.
Adam Gainski
10 January, 2026I work with a lot of elderly patients on these meds. The real issue isn’t just which drug works better-it’s who can stick with it. Abaloparatide has lower discontinuation rates because of fewer side effects, but cost blocks access. Insurance step therapy is broken. If you’re on teriparatide and doing okay, don’t switch just because the new one looks shinier.
Katrina Morris
11 January, 2026my dr just gave me the teriparatide script and i was so scared but reading this made me feel better like maybe its not the end of the world if i cant afford the other one
Mina Murray
11 January, 2026Funny how the same people who scream about drug prices are the ones who never check if their insurance even covers the cheaper option. Teriparatide’s generic now-so why are you still paying $5k for abaloparatide? Someone’s getting played here.
Emma Addison Thomas
12 January, 2026I'm from the UK and we don't even get abaloparatide on the NHS unless you've had two fractures. Teriparatide is the only option for most. It's frustrating when the science says one thing and the system says another. I wish we had more access to the better drug, but we make do.
Andrew N
12 January, 2026The 17% lower hip fracture rate with abaloparatide is only in observational data. The ACTIVE trial wasn't powered for that endpoint. Don't overinterpret real-world studies-they're noisy.