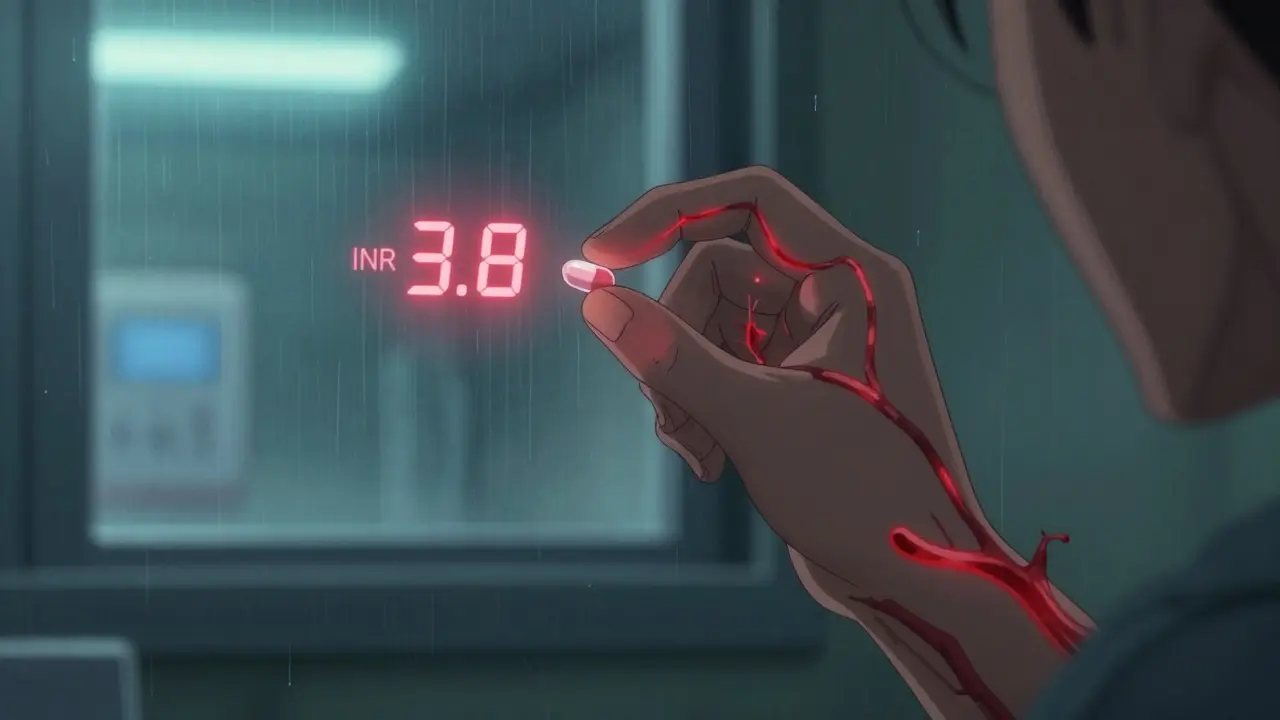
Switching from brand-name Coumadin to a generic version of warfarin might seem like a simple cost-saving move - and for most people, it is. But this isn’t like swapping one brand of ibuprofen for another. Warfarin is a warfarin drug with a razor-thin margin between working and causing harm. One wrong dose, one unexpected interaction, one switch in manufacturer - and your INR can swing out of range. That’s not a hypothetical risk. It’s a real, documented danger that has sent people to the ER with internal bleeding or triggered strokes because a clot formed when their blood was too thin. You might think: "If the FDA says they’re equivalent, why worry?" The truth is, bioequivalence standards for warfarin don’t guarantee identical effects in every person. The FDA requires generic versions to match the brand in how much drug enters your bloodstream (AUC) and how fast it peaks (Cmax), within 80-125%. Sounds tight, right? But for a drug where the difference between 2.0 and 3.0 INR can mean life or death, even small shifts matter. And not all generics are made the same - different fillers, coatings, and manufacturing processes can subtly change how your body absorbs the pill. A 2000 study of 182 patients in a St. Louis HMO found no increase in bleeding or clotting after switching from Coumadin to a single generic brand (Barr Laboratories). That’s reassuring. But here’s what didn’t make headlines: 15-20% of those patients had noticeable INR changes in the first few weeks. Some went from rock-stable at 2.5 to 3.8 in just five days. Others dropped to 1.6. No symptoms. No warning. Just numbers on a lab sheet. That’s why experts don’t say "switch and forget." They say: switch and watch closely.
When You Switch, Monitor More - Not Less
If you’ve been on Coumadin for years and your doctor switches you to a generic, don’t assume your routine INR checks (every 6 weeks) are enough. The Cleveland Clinic, the American Family Physician, and the College of American Pathologists all agree: after switching, you need daily or every-other-day INR tests for at least 1-2 weeks. Only after two consecutive readings stay in your target range should you go back to monthly checks. Why so often? Because warfarin’s effect builds slowly. It takes 3-5 days for a dose change to fully show up in your INR. If you switch pills on Monday and your INR spikes on Thursday, you won’t know if it’s the new generic, a change in your broccoli intake, or an antibiotic you took for a cold. Daily testing gives you the data to untangle it. And don’t wait for your doctor to suggest it. If you’re switched to a new generic and your next INR is scheduled for 4 weeks from now - push back. Ask for a test in 3-5 days. Your life isn’t worth the delay.What Your INR Target Should Be
Not everyone’s target is the same. If you have atrial fibrillation or a blood clot in your leg, your goal is usually 2.0-3.0. But if you have a mechanical heart valve - especially in the mitral position - your target is higher: 2.5-3.5. For some high-risk aortic valves, it’s 3.0-4.0. That’s not a suggestion. That’s a safety zone. If your INR drops below 2.0 with a mechanical valve, you’re at risk of a clot forming on the valve. That clot can break loose and cause a stroke. If it goes above 4.0, even a minor bump can lead to bleeding in your brain or gut. And here’s the scary part: you might not feel a thing until it’s too late. That’s why knowing your target is non-negotiable. Write it down. Keep it on your phone. Tell your family. If you’re switched to a new generic and your INR starts drifting, you need to know whether it’s just a blip or a red flag.What Can Throw Your INR Off - Even Without Switching
Warfarin doesn’t live in a vacuum. It’s sensitive to almost everything you put in your body. Food: Vitamin K counteracts warfarin. If you suddenly start eating a lot of kale, spinach, broccoli, or Brussels sprouts - your INR will drop. Go cold turkey on greens? Your INR can spike. The key isn’t to avoid these foods - it’s to keep your intake consistent. Don’t eat 3 cups of spinach every day one week and zero the next. Aim for 100-150 mcg of vitamin K daily, and stick to it. Medications: Over 300 drugs interact with warfarin. Antibiotics like trimethoprim-sulfamethoxazole? Can double your INR. Painkillers like ibuprofen or naproxen? Increase bleeding risk. Even some herbal supplements - garlic, ginkgo, green tea extract - can interfere. Always check with your pharmacist before starting anything new, even OTC. Alcohol: Heavy drinking raises your INR. A glass of wine with dinner? Usually fine. A six-pack on Saturday? That’s a risk. Illness: If you get the flu, an infection, or even severe diarrhea, your liver may process warfarin differently. Your INR can swing wildly. That’s why you need to call your anticoagulation clinic if you’re sick - don’t wait for your next scheduled test.Why Some People Struggle After Switching - And What to Do
About 80% of patients transition to generic warfarin without issue. But 15-20%? They get unpredictable INR results. Not because the generic is bad. But because their body reacts differently to the new formulation. If your INR jumps or drops unexpectedly after switching - and you haven’t changed your diet, meds, or habits - the first thing to do is not panic. The second thing? Don’t adjust your dose yourself. Call your anticoagulation provider. They’ll likely:- Check your INR again in 24-48 hours
- Ask about recent changes (even small ones - like a new laundry detergent or vitamin you started)
- Review your pill bottle to confirm the manufacturer and lot number
- Consider switching back to your old generic or brand if the instability continues
Warfarin vs. DOACs: The Real Trade-Off
You’ve probably heard about the new anticoagulants - apixaban, rivaroxaban, dabigatran. DOACs. They don’t need INR checks. No blood tests. No dietary restrictions. They’re easier. And they’re more expensive. Generic warfarin costs $4-$10 a month. DOACs? $300-$500. That’s why millions of people - especially those on Medicare - still take warfarin. But here’s the catch: DOACs are safer for most people. They cause fewer brain bleeds. Fewer GI bleeds. And you don’t have to live with the anxiety of wondering if your INR is off. So why not switch to a DOAC? Because they’re not for everyone. If you have a mechanical heart valve, DOACs don’t work. If you have severe kidney disease, many DOACs are unsafe. And if you’re on a tight budget? Warfarin is still the only affordable option. The choice isn’t just about cost. It’s about lifestyle. Can you handle monthly blood tests? Do you remember to take your pill at the same time every day? Are you okay with eating the same amount of greens every week? If yes - warfarin is fine. If no - talk to your doctor about DOACs.What You Can Do Right Now
If you’re on warfarin - whether brand or generic - here’s your action plan:- Know your target INR. Write it down. Keep it with your meds.
- If you’re switched to a new generic, ask for INR checks every 2-3 days for the first week, then weekly until stable.
- Keep a food log. Track your vitamin K intake. Don’t guess - measure.
- Never start a new medication, supplement, or herb without checking with your anticoagulation clinic.
- Always carry a card in your wallet that says: "I take warfarin. My INR target is [X]. Emergency contact: [Name/Number]."
- Ask your pharmacist: "Which manufacturer’s warfarin am I getting?" Keep a note of it.
Frequently Asked Questions
Can I switch between different generic warfarin brands without risk?
Switching between different generic manufacturers - say, from Teva to Mylan - can cause INR changes, even if both are FDA-approved. The FDA says all generics are "therapeutically equivalent," but that doesn’t mean identical in every person. If you’re switched to a new generic, expect closer monitoring for 1-2 weeks. Never switch manufacturers without telling your anticoagulation clinic.
Is generic warfarin less effective than Coumadin?
No. Large studies show that, on average, generic warfarin works just as well as Coumadin. But "on average" doesn’t mean "for everyone." About 1 in 5 people experience INR shifts after switching. That’s not because the drug is weaker - it’s because individual biology responds differently to small formulation changes. The key is monitoring, not brand loyalty.
Why does my INR change when I travel or change time zones?
Warfarin’s effect depends on consistent dosing and metabolism. Time zone changes can disrupt your routine - you might miss a dose, take it late, or eat differently. Jet lag also affects liver function. If you’re traveling, plan ahead. Get an INR check before you leave. Bring extra pills. Avoid alcohol and new foods. And if you’re gone longer than a week, arrange for a local blood test.
Should I get genetic testing for warfarin sensitivity?
Genetic testing for CYP2C9 and VKORC1 genes can predict how your body processes warfarin. It’s not routine - but if you’ve had multiple unexplained INR swings, or if you’re starting warfarin and have a history of bleeding, it’s worth discussing. Some clinics now use it to guide initial dosing. It won’t prevent all issues, but it can reduce the number of dose adjustments needed early on.
What should I do if my INR is dangerously high or low?
If your INR is above 5.0 and you’re not bleeding, your provider may hold your dose and give you vitamin K. If it’s above 8.0, you may need urgent treatment. If your INR is below 1.5 and you have a mechanical valve, you’re at risk of clotting - contact your clinic immediately. Never adjust your dose yourself. Call your provider. If you’re bleeding (bruising without cause, blood in urine, black stools, severe headache), go to the ER - don’t wait.

14 Comments
Ryan W
26 January, 2026Let’s cut through the noise: if you’re on warfarin, you’re not a patient-you’re a lab rat with a pill schedule. The FDA’s 80-125% bioequivalence window is a joke when your INR swings from 2.1 to 3.9 because Teva swapped out corn starch for lactose. I’ve seen three guys in my VA clinic end up in the ER over this. No one’s talking about the real issue: generics aren’t interchangeable. They’re pharmaceutical Russian roulette. And yes, I know the study says ‘no difference.’ But my INR didn’t get the memo.
Allie Lehto
26 January, 2026i just switched to generic and my INR went crazy 😭 i cried in the pharma line bc i thought i was gonna die. i eat kale every day but now i’m scared of spinach. why does my body hate me?? 🥲 i just want to live without checking my blood every 3 days. #warfarintrauma
Henry Jenkins
28 January, 2026There’s a deeper layer here that the article barely touches: warfarin isn’t just a drug-it’s a mirror of our healthcare system’s fragmentation. We allow patients to be shuffled between manufacturers like inventory, without tracking formulation changes at the individual level. We don’t have a national registry for anticoagulant exposure. We don’t require pharmacists to flag generic switches in EHRs. We treat a life-threatening medication like a box of aspirin. The science is sound, but the infrastructure is broken. And until we fix that, the ‘15-20%’ aren’t outliers-they’re the canaries in the coal mine.
Dan Nichols
30 January, 2026Everyone’s freaking out about generics but no one’s talking about the real villain-the anticoagulation clinics that charge $80 per INR test and make you wait 3 weeks for an appointment. If your INR’s off, you’re supposed to call them but good luck getting through. Meanwhile, the pharmacy gives you a new bottle with no warning. The system’s rigged. And don’t even get me started on DOACs-$500 a month? That’s not healthcare, that’s corporate extortion. Warfarin’s cheap because it’s old. But we treat it like it’s disposable. That’s the real problem.
Renia Pyles
31 January, 2026Ugh. Another ‘educational’ post from someone who clearly never had to explain to their 82-year-old grandma why she can’t eat a salad anymore. You talk about ‘monitoring’ like it’s a chore. It’s a full-time job. My mom’s on warfarin, she’s got dementia, and the last time she switched generics, she took two pills by accident because the color changed. She bled into her knee. We had to go to the ER. And now you want me to believe this is just ‘bioequivalence’? Wake up. This isn’t science-it’s negligence dressed up in jargon.
George Rahn
1 February, 2026Let us not forget the grand irony of American medicine: we champion innovation, yet we treat the most dangerous anticoagulant in history as a commodity to be commoditized. The FDA’s regulatory framework was designed for aspirin-not for a drug where a 0.5 INR shift can mean hemorrhagic stroke. We have the technology to track genetic polymorphisms, to log batch-specific formulations, to integrate real-time INR data into AI-driven dashboards. But we don’t. Why? Because profit margins on warfarin are too thin to justify investment. We are not failing because of science-we are failing because of capitalism. And until we acknowledge that, patients will continue to bleed out in silence.
Napoleon Huere
3 February, 2026Warfarin is a metaphor for human fragility. We are all balancing on a razor’s edge-between safety and catastrophe, between control and chaos. The pill is just a tool. The real question is: do we have the humility to recognize that our bodies are not machines, and that biology refuses to be standardized? We want to reduce everything to numbers-INR, AUC, Cmax-but life is messy. A change in sleep. A bad day. A new laundry detergent. These things matter. And if we keep pretending that a pill is just a pill, we’re not just ignoring science-we’re ignoring the soul of medicine.
Aishah Bango
4 February, 2026I’m a nurse. I’ve seen this too many times. A patient gets switched to a new generic. No warning. No education. Then they come in with a subdural hematoma because their INR was 6.8 and they thought ‘it’s just a different brand.’ You can’t just hand someone a pill and say ‘you’re fine.’ You need to sit with them. Explain. Show them the color change. Tell them to call if they feel dizzy. But no one has time. And that’s not the patient’s fault. It’s the system’s.
Simran Kaur
5 February, 2026In India, we use warfarin too-but we don’t have the luxury of daily INR tests. Many people get their blood checked only once a month, if they’re lucky. But here’s what we do: we teach families to watch for signs-dark stools, headaches, unexplained bruising. We make sure the patient carries a note in Hindi and English. We don’t wait for the system to fix itself-we fix it ourselves. Maybe the answer isn’t more technology. Maybe it’s community. Maybe it’s love.
Neil Thorogood
7 February, 2026Bro. I switched to generic warfarin last year. Did I panic? Nah. Did I call my clinic? Hell yeah. Did I track my vitamin K like it was my job? 😎 Yep. I even made a spreadsheet. 📊 And guess what? My INR stayed perfect. You don’t need a PhD to manage this. You need discipline. And a little bit of sass. Warfarin’s not magic. It’s math. Do the math. Don’t be lazy. 💪 #WarfarinWarrior
Jessica Knuteson
8 February, 2026INR targets are arbitrary. The 2.0-3.0 range? Based on 1980s trials. Mechanical valve targets? Even less evidence. We treat these numbers like gospel but they’re just averages. You’re not a number. You’re a person. And if your body hates a certain generic, you should be able to demand the one that works. But insurance won’t cover it. So you suffer. Welcome to modern medicine.
Robin Van Emous
10 February, 2026I just want to say thank you to the person who wrote this. I’ve been on warfarin for 12 years. I’ve switched generics four times. I’ve had scary INR spikes. But I’ve also learned how to listen to my body. I keep a food journal. I call my clinic before I take any new pill. I tell my kids what to do if I collapse. This isn’t about fear. It’s about responsibility. And if we all did a little more of this, fewer people would end up in the ER. You’re not alone. We’re all in this together.
Angie Thompson
11 February, 2026Y’all are overcomplicating this. Warfarin? It’s just like riding a bike. You don’t need to be a genius-you just need to be consistent. Same food. Same time. Same pill. Same routine. I switched from Coumadin to Teva last year. My INR? Perfect. I even started hiking. I’m 70 and I feel great. Don’t let fear scare you out of saving $400 a month. You got this. 🌞💪 #WarfarinLife
SWAPNIL SIDAM
12 February, 2026Back home in India, we use warfarin because we can’t afford DOACs. But we don’t switch generics lightly. My uncle was on one brand for 8 years. When they changed it, his INR went wild. We took him to a private lab. Paid out of pocket. He’s fine now. I wish more people knew: in poor countries, we don’t wait for the system to fix itself. We fix it ourselves. One pill. One test. One life at a time.