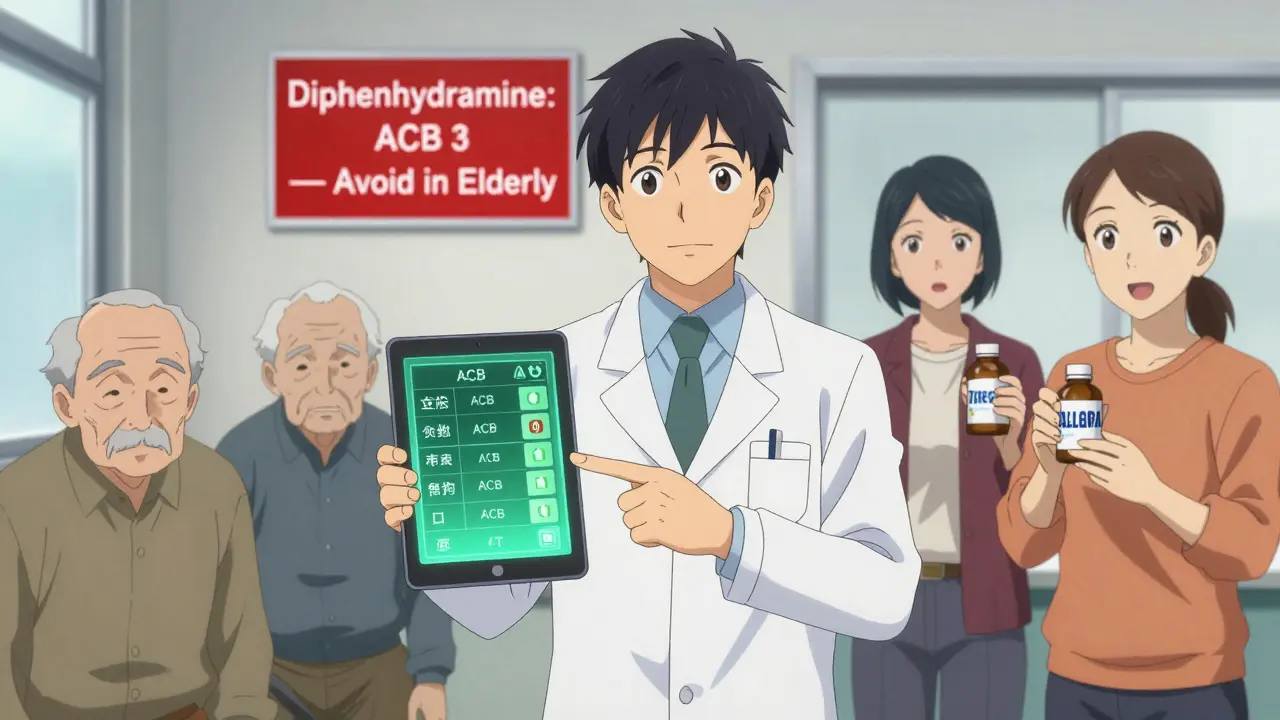
Anticholinergic Burden Calculator
How This Calculator Works
This tool calculates your total Anticholinergic Burden (ACB) score based on medications you take. Higher scores indicate greater risk of confusion, memory problems, and falls, especially in older adults. ACB Scale:
- 0: No anticholinergic burden
- 1: Low burden
- 2-3: Moderate to high burden
Combining antihistamines with other sedating medications can be dangerous - and many people don’t realize it until it’s too late. If you’re taking something like Benadryl for allergies, a sleep aid, or even motion sickness, and you’re also on a benzodiazepine, opioid, or sleep medication, you could be putting yourself at serious risk. The problem isn’t just drowsiness. It’s slowed breathing, confusion, falls, hospital visits, and in older adults, even delirium or long-term cognitive decline.
Why First-Generation Antihistamines Are Risky
Not all antihistamines are the same. The ones you can buy over the counter - diphenhydramine (Benadryl), hydroxyzine, and promethazine - are called first-generation antihistamines. They work quickly, but they also cross into your brain. That’s why they make you sleepy. But that same brain penetration is what makes them dangerous when mixed with other sedating drugs.These medications have strong anticholinergic effects. That means they block acetylcholine, a key chemical in your nervous system. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3 - the highest level. That’s worse than many prescription sedatives. When you add it to another anticholinergic drug, like oxybutynin for overactive bladder, your risk of confusion and memory problems jumps by 54%, according to a 2021 JAMA Internal Medicine study.
Even worse, your body clears these drugs slower as you age. People over 65 clear diphenhydramine 50-70% slower than younger adults. That means even a normal dose can build up to toxic levels over time, especially if you’re taking multiple medications.
What Medications Should You Avoid Mixing With Them?
First-generation antihistamines don’t just make you drowsy - they amplify the effects of other CNS depressants. Here’s what to watch out for:- Benzodiazepines (like lorazepam, alprazolam): Combining these with diphenhydramine increases sedation by up to 42% in clinical studies. One Reddit user reported nearly dying after mixing 50mg of Benadryl with 1mg of Xanax.
- Opioids (like oxycodone, hydrocodone): The CDC found that combining opioids with first-gen antihistamines raises the risk of respiratory depression from 1.5% to 8.7%. WebMD users report 41% experienced severe dizziness requiring ER visits.
- Alcohol: Even one drink with 25mg of diphenhydramine has led to blackouts and hospitalizations, according to BuzzRx data.
- Sleep medications (like zolpidem): These are designed to slow your brain. Adding an antihistamine pushes that effect into dangerous territory.
- Cimetidine (Tagamet): This H2 blocker doesn’t cause sedation, but it shuts down liver enzymes that break down diphenhydramine. That can cause levels to spike 40-70%, increasing side effects.
These aren’t rare events. In 2022, the FDA recorded 2,847 adverse events linked to antihistamine interactions. Emergency departments saw over 300,000 visits that year for CNS depressant reactions - and antihistamines were involved in nearly 15% of them.
Second-Generation Antihistamines Are the Safer Choice
If you need an antihistamine, you have a much safer option: second-generation drugs like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra). These were designed to stay out of your brain. They use special transporters to block entry into the central nervous system.That means they don’t cause the same level of drowsiness. GoodRx surveys show 97% of users report no drowsiness with loratadine, compared to 68% with diphenhydramine. Amazon reviews for Allegra sit at 4.3 out of 5 stars, with users praising its lack of interaction with other meds. Benadryl? Only 2.9 out of 5, with 68% of negative reviews citing dangerous drowsiness.
Second-gen antihistamines also have low ACB scores - usually 0 or 1. That means they don’t add to your overall anticholinergic burden. Even cetirizine, which scores a 1, is far safer than diphenhydramine’s 3. And newer options like bilastine show no interaction with benzodiazepines even at high doses, according to a 2023 study in the Journal of Clinical Psychopharmacology.

Why Do People Still Use the Risky Ones?
It’s not because they’re more effective. It’s because they’re cheap, widely available, and marketed as sleep aids. Many older adults use diphenhydramine to help them fall asleep - not realizing it’s not a true sleep medication. It’s a sedative that disrupts sleep architecture, leaving you with poor-quality rest.Doctors used to prescribe these routinely. But that’s changing. The American Geriatrics Society added first-gen antihistamines to its Beers Criteria in 2023 - a list of medications that should be avoided in older adults. The FDA now requires bold warnings on diphenhydramine packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.”
Market trends confirm the shift. First-gen antihistamine sales have dropped 12.7% yearly since 2018. Second-gen drugs now make up 83% of the $2.4 billion U.S. OTC antihistamine market. Over 78% of allergists now start patients on loratadine or cetirizine - up from just 52% in 2015.
What Should You Do If You’re Taking Both?
If you’re on a first-generation antihistamine and another sedating drug, don’t stop suddenly. Talk to your doctor or pharmacist. Here’s what to ask:- Is this antihistamine necessary? Could I switch to loratadine or fexofenadine?
- What’s my total anticholinergic burden? (Use the University of Washington’s free ACB calculator.)
- Am I taking three or more medications with ACB scores of 1 or higher? If so, deprescribing first-gen antihistamines is strongly recommended.
Pharmacists can run interaction checks using tools from the Institute for Safe Medication Practices. Many hospitals now have automated alerts that flag these combinations before a prescription is filled. Kaiser Permanente’s system cut antihistamine-related adverse events by 34% between 2020 and 2022.
Special Cases: When First-Gen Might Still Be Used
There are a few exceptions. Dimenhydrinate (Dramamine), which contains diphenhydramine, is still the go-to for motion sickness. Some palliative care teams use low-dose diphenhydramine with benzodiazepines to manage terminal agitation - but only under close supervision.These are narrow exceptions. For 99% of people - especially those over 50 or on multiple medications - the risks far outweigh the benefits.
What’s Next? The Future of Antihistamines
The next wave of antihistamines - like levocetirizine (Xyzal) - are even more targeted. They bind only to H1 receptors and avoid off-target effects. Pharmacogenomic testing is starting to show that people with certain gene variants (like CYP2D6 poor metabolizers) break down diphenhydramine extremely slowly, making them far more vulnerable to overdose.By 2028, experts predict first-gen antihistamines will make up less than 22% of the market. They’ll likely be restricted to specific uses like motion sickness or short-term sedation in controlled settings. For everyday allergies, sleep, or cold symptoms, second-generation options are now the standard.
Can I take Benadryl with my anxiety medication?
No. Combining diphenhydramine (Benadryl) with benzodiazepines like Xanax or lorazepam can cause extreme drowsiness, confusion, and even slowed breathing. A 2013 study showed diphenhydramine increased lorazepam’s sedative effects by 37%. Use loratadine or cetirizine instead - they don’t interact the same way.
Is Zyrtec safer than Benadryl?
Yes. Zyrtec (cetirizine) is a second-generation antihistamine with minimal brain penetration. It’s much less likely to cause drowsiness or interact dangerously with other sedatives. While it has a low ACB score of 1, it’s still far safer than Benadryl’s score of 3. For most people, Zyrtec is the better choice.
Why do doctors still prescribe diphenhydramine?
Some doctors still prescribe it out of habit, or because it’s cheap and available without a prescription. But guidelines have changed. The American Geriatrics Society now says first-gen antihistamines should be avoided in older adults. Most allergists now start with second-generation options. If you’re prescribed diphenhydramine, ask if a safer alternative is available.
Can antihistamines cause dementia?
Long-term use of high-anticholinergic drugs - including diphenhydramine - has been linked to a 54% increased risk of dementia, according to a 2015 study in JAMA Internal Medicine. The risk builds up over time, especially in older adults taking multiple anticholinergic medications. Switching to low-ACB antihistamines reduces this risk.
What should I do if I feel too drowsy after taking an antihistamine?
Stop taking it and talk to your doctor. If you’re also on opioids, sleep aids, or alcohol, seek medical attention immediately. Severe drowsiness combined with slow breathing could signal respiratory depression - a life-threatening condition. Keep a list of all your medications and bring it to every appointment.


11 Comments
Anna Giakoumakatou
17 December, 2025Oh, so we're just now realizing that giving grandma a Benadryl lollipop before her bingo night is a one-way ticket to delirium town? Groundbreaking. I'm sure the pharmaceutical reps didn't bribe her doctor with free samples of this neurotoxic glitter.
Meanwhile, the FDA is still playing whack-a-mole with warning labels while the anticholinergic fog rolls over our nursing homes like a slow, sedated tsunami. At least the ACB scale has a score - unlike our collective will to change.
And let’s not forget: the real tragedy isn’t the drug interaction - it’s that we still treat aging like a bug to be medicated instead of a biological process to be respected.
But hey, at least we’ve got Zyrtec now. And by ‘we,’ I mean the people who can afford $12 for a bottle of non-sedating antihistamine while the rest of us are still scraping diphenhydramine off the bottom of the cupboard like it’s a relic from the 1980s.
Progress? More like rearranging deck chairs on the Titanic… with a side of cognitive decline.
Someone call the Beers Criteria. And maybe a therapist for the geriatricians still prescribing this like it’s a lullaby.
CAROL MUTISO
17 December, 2025Wow. This post reads like a love letter to pharmacology nerds - and honestly? I’m here for it.
I used to pop Benadryl like candy when I had seasonal allergies, thinking ‘hey, it’s just a sleep aid.’ Then I started mixing it with my low-dose Xanax because ‘I just need to chill.’ Spoiler: I didn’t chill. I nearly passed out on my kitchen floor while trying to make tea.
Switched to cetirizine. Zero drowsiness. Zero brain fog. Zero ER visits. My brain feels like it’s been unplugged from a 1990s dial-up modem.
And yes - the ACB scale is terrifying. I printed mine out and taped it to my medicine cabinet. My pharmacist laughed. Then she gave me a free sample of fexofenadine. We’re both weird, but we’re alive.
If you’re over 50 and still using diphenhydramine for sleep, please - for the love of all that is neurochemically sound - talk to someone. Your future self will thank you. And no, ‘I’ve been doing it for 20 years’ doesn’t make it safe. It just makes you a walking case study.
Erik J
18 December, 2025Interesting data. I’m curious about the pharmacokinetics in CYP2D6 poor metabolizers - the study mentioned but didn’t cite. Is there a specific allele frequency in the U.S. population that makes this risk more prevalent in certain ethnic groups?
Also, the 54% increased dementia risk - was that adjusted for polypharmacy? I ask because many of these patients are also on statins, anticholinergic antidepressants, and bladder meds. Is the antihistamine the main driver, or just one component of a cumulative burden?
And why is dimenhydrinate still considered acceptable for motion sickness? Is it because the exposure is short-term, or is there a different mechanism at play?
I’d love to see a breakdown of adverse event reports by age group and concomitant meds. The FDA data seems too broad to be actionable without stratification.
BETH VON KAUFFMANN
18 December, 2025Let’s be real - this is just another fearmongering op-ed dressed up as clinical guidance. The data is cherry-picked. You cite JAMA, but ignore the 2019 meta-analysis in BMJ that found no significant association between short-term antihistamine use and dementia.
Also, ‘second-gen antihistamines are safer’? Cetirizine has a 1 on the ACB scale. It’s not zero. And it still causes sedation in 15% of users - same as loratadine in some populations.
And who’s telling you to stop your meds? Not your doctor? Then why are you reading Reddit? Go to a pharmacist. Or better yet - stop Googling your symptoms and trust your provider.
Also, ‘Benadryl has 2.9 stars’? That’s because people don’t understand how antihistamines work. It’s not a sleep drug. It’s an anticholinergic. If you take it to sleep, you’re doing it wrong. Not the drug’s fault.
Stop the panic. Start the education. And for god’s sake, stop conflating correlation with causation.
Martin Spedding
20 December, 2025benadryl + xanax = death. i know. i did it. woke up in the er with my mom screaming. no joke. they had to pump my stomach. i was 22.
now i take claritin. no drama. no hospital. no near-death experience. just… chill.
also cimetidine is a sneaky bastard. nobody talks about it. but it’ll kill you slow. like a slow-mo car crash in your liver.
ps: i typed this on my phone. sorry for typos. brain still fuzzy from last year.
Raven C
21 December, 2025How utterly… distressing. To think that our healthcare system still permits such reckless pharmacological negligence to persist under the guise of ‘over-the-counter convenience.’
One must wonder - is this not a moral failure? A societal abandonment of geriatric dignity? To allow a substance with an ACB score of 3 - equivalent, in some circles, to the cognitive burden of early-stage Alzheimer’s - to be sold alongside candy and gum?
And the marketing! The predatory, insidious marketing that positions sedation as ‘rest.’ As if sleep were a commodity to be bought with neurochemical suppression.
I refuse to believe that the human intellect has not evolved beyond this. We have the science. We have the data. We have the guidelines. And yet - we continue to allow our elders to be chemically muzzled, as if their minds were disposable.
Where is the outrage? Where is the legislation? Where is the shame?
Donna Packard
22 December, 2025I’m so glad someone finally put this out there. My mom took Benadryl for years for sleep - she didn’t even realize it was making her more confused. We switched her to Zyrtec and her memory improved in just a few weeks. She started remembering names again.
It’s not just about avoiding bad reactions - it’s about preserving who you are. Your thoughts. Your memories. Your sense of self.
If you’re reading this and you’re on diphenhydramine - please, talk to your doctor. Don’t wait for a fall, or a blackout, or a hospital visit. You deserve to feel clear-headed. You deserve to sleep well - not just be knocked out.
Small change. Big difference.
Patrick A. Ck. Trip
23 December, 2025Thank you for this comprehensive and well-researched overview. The data presented aligns closely with current clinical guidelines from the American Geriatrics Society and the Institute for Safe Medication Practices.
I have personally counseled over 30 elderly patients who were unknowingly on multiple anticholinergic agents - and in nearly every case, replacing first-generation antihistamines with second-generation alternatives resulted in measurable improvements in cognitive clarity and functional independence.
It is imperative that healthcare providers, pharmacists, and patients engage in proactive deprescribing conversations. Automated alerts in EHR systems, such as those implemented at Kaiser Permanente, are a vital step forward.
May we continue to prioritize patient safety over convenience - and science over tradition.
With gratitude and respect,
P.A.C. Trip
Sam Clark
25 December, 2025This is exactly the kind of information that needs to be shared more widely. I work as a pharmacy tech and see this exact interaction every week - especially with older patients who think Benadryl is ‘just a sleep aid.’
My advice to anyone reading this: Make a list of every medication and supplement you take - including OTC stuff - and bring it to your next appointment. Don’t assume your doctor knows what you’re taking. Don’t assume your pharmacist caught it. Be your own advocate.
Switching to Claritin or Allegra isn’t a sacrifice - it’s a upgrade. Your brain will thank you. Your family will thank you. And you’ll probably sleep better, too - because real sleep doesn’t come from being drugged.
You’ve got this.
Jessica Salgado
26 December, 2025I cried reading this.
My dad had a fall last year. They thought it was just old age. Turns out, he’d been taking Benadryl for ‘sleep’ for 15 years - plus his blood pressure med, his anxiety med, and his bladder pill. All anticholinergic. All stacking up. His ACB score? 7. Seven.
He didn’t have dementia. Not yet. But he was confused. He forgot my name once. Just once. And I’ll never forget how it felt.
We switched him to loratadine. Three months later, he remembered my birthday. He remembered my dog’s name. He started reading again.
This isn’t just about drugs. It’s about identity. It’s about dignity.
Don’t wait until it’s too late.
Please. Just… talk to someone.
Linda Caldwell
27 December, 2025Just switch to Zyrtec and stop stressing. Your brain will thank you.