For many people, a stuffy nose that won’t go away isn’t just annoying-it’s exhausting. If you’ve had nasal congestion, facial pressure, or a lost sense of smell for more than three months, you’re not just dealing with a bad cold. You might have chronic sinusitis. Unlike acute sinusitis, which clears up in a couple of weeks, chronic sinusitis lingers. And it’s more common than you think: about 9% of people worldwide deal with it every year. In the U.S. alone, 31 million people are diagnosed annually. Most of them aren’t sick because of a lingering infection. They’re stuck in a cycle of inflammation, blocked drainage, and irritation that won’t resolve with antibiotics alone.
What Exactly Is Chronic Sinusitis?
Chronic sinusitis, also called chronic rhinosinusitis, means your sinuses-the hollow spaces in your forehead, cheeks, and nose-are swollen and inflamed for 12 weeks or longer, even with treatment. It’s not one disease. It’s a group of conditions with similar symptoms but different causes. The main ones are: chronic sinusitis without nasal polyps, chronic sinusitis with nasal polyps, and allergic fungal rhinosinusitis. Each needs a slightly different approach.
Doctors diagnose it when you have at least two of these symptoms for 12 weeks or more: blocked nose, thick nasal discharge (either dripping out or down the back of your throat), facial pain or pressure, and reduced or lost sense of smell. A physical exam might show pus or polyps. But the real confirmation comes from a nasal endoscopy (a thin camera inserted into your nose) or a CT scan that shows thickened sinus lining.
Why Do You Get It? Allergies, Irritants, and Structural Issues
Most people assume chronic sinusitis is caused by a bacterial infection. It’s not. Only about 30% of cases involve active bacteria. The rest? It’s inflammation.
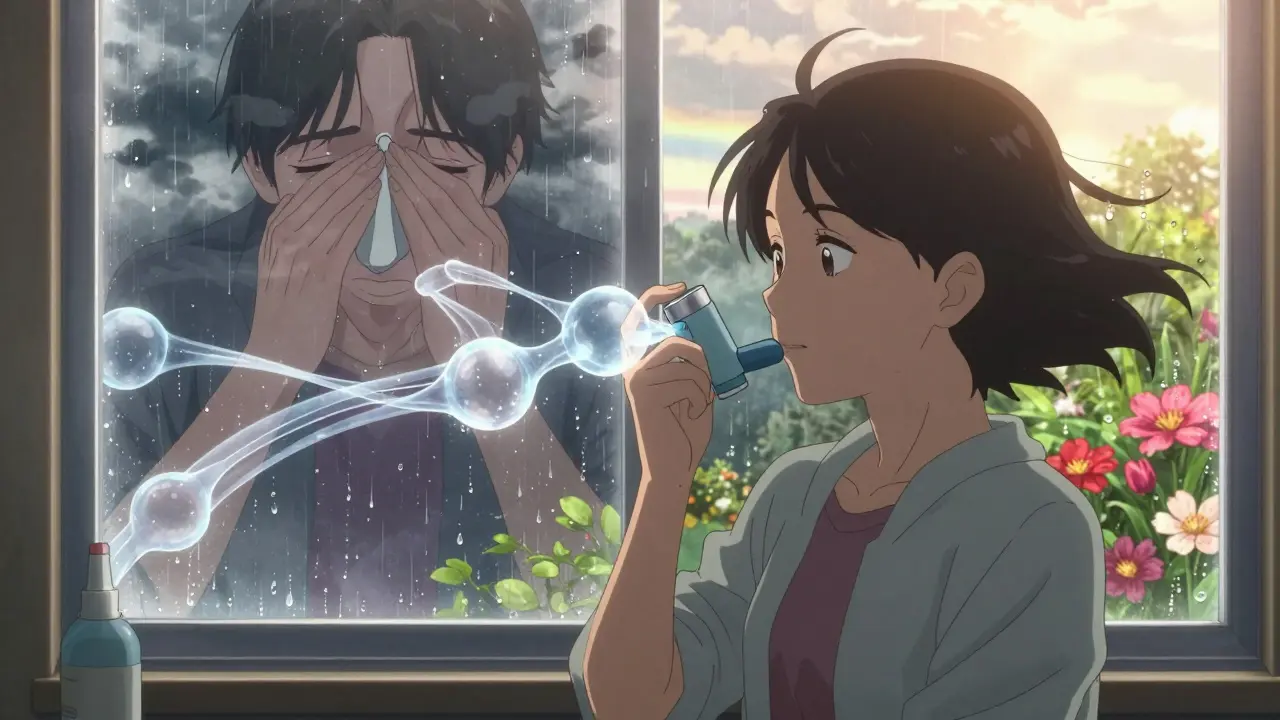
Allergies are a big trigger. If you have hay fever, pet dander sensitivity, or dust mite allergies, your risk of chronic sinusitis goes up by 2.5 times. Asthma makes it even worse-people with asthma are 3 to 4 times more likely to develop it. That’s because your airways, from your nose to your lungs, share the same inflammatory pathways.
Nasal polyps-soft, noncancerous growths inside your nose-are present in 25-30% of chronic sinusitis cases. They’re like little balloons of swollen tissue that block airflow and mucus drainage. And if you have polyps plus asthma and sensitivity to aspirin (called Samter’s triad), your case is often harder to treat.
Environmental irritants matter too. Smoking, secondhand smoke, air pollution, and even dry air can worsen inflammation. One study found that exposure to tobacco smoke increases your risk by 35%. If you live in a dry climate like parts of Australia or the U.S. Southwest, low humidity can dry out your nasal passages, making them more prone to irritation.
Structural problems play a role too. A deviated septum, narrow sinus openings, or enlarged turbinates can physically block drainage. These aren’t always obvious without imaging. That’s why a CT scan is often needed-not to find an infection, but to see if your anatomy is working against you.
First-Line Treatment: Saline and Steroids
Before you think about surgery or strong medications, start with the basics. The most effective first step for almost everyone is daily nasal saline irrigation. It’s cheap, safe, and works. You use a neti pot or squeeze bottle with sterile saltwater to flush out mucus, allergens, and irritants. Studies show this alone improves symptoms in up to 70% of people.
Next comes intranasal corticosteroid sprays. These aren’t the same as the steroids athletes use. These are local, targeted anti-inflammatories. Brands like Flonase (fluticasone), Rhinocort (budesonide), and Nasonex (mometasone) reduce swelling in your sinuses. They don’t work overnight. It takes 4 to 8 weeks of daily use to see real improvement. But once they kick in, 60-70% of patients get significant relief.
Here’s the catch: most people stop using them too soon. Only about 60% stick with the spray long-term because of the initial burning sensation or because they don’t feel better right away. But skipping doses or quitting early is why so many people end up thinking their treatment “didn’t work.” Consistency is everything.
What About Allergies and Antibiotics?
If allergies are driving your sinusitis, antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) can help. They’re not a cure, but they reduce the allergic response that triggers swelling. Studies show they cut symptoms by 45-60% in allergic patients.
Antibiotics? Don’t expect much. The American Academy of Allergy, Asthma & Immunology says antibiotics usually don’t help in chronic cases because bacteria aren’t the main problem. If you’ve had a flare-up with thick yellow-green mucus and fever, your doctor might try a 21-28 day course of amoxicillin-clavulanate. But if symptoms return after finishing the antibiotics, it’s not an infection-it’s inflammation. Keep using your steroid spray.
When Medication Isn’t Enough: Biologics for Severe Cases
If you’ve tried nasal sprays, saline, and antihistamines for months and still can’t breathe, smell, or sleep, you might be a candidate for biologic therapy. These are injectable drugs that target specific parts of your immune system.
Dupilumab (Dupixent) was approved by the FDA in 2019 specifically for chronic sinusitis with nasal polyps. In clinical trials, it reduced polyp size by 50-60% and improved breathing and smell in 30-40% of patients. It’s not cheap-it’s given as a shot every two weeks-but for people who’ve failed everything else, it’s life-changing.
Other biologics like omalizumab (Xolair) and mepolizumab (Nucala) are also being used off-label with 35-55% success rates. These are typically reserved for patients with severe polyps, asthma, or Samter’s triad. They’re not for mild cases. But for those who qualify, they can mean avoiding surgery entirely.
Surgery: When and What Kind?
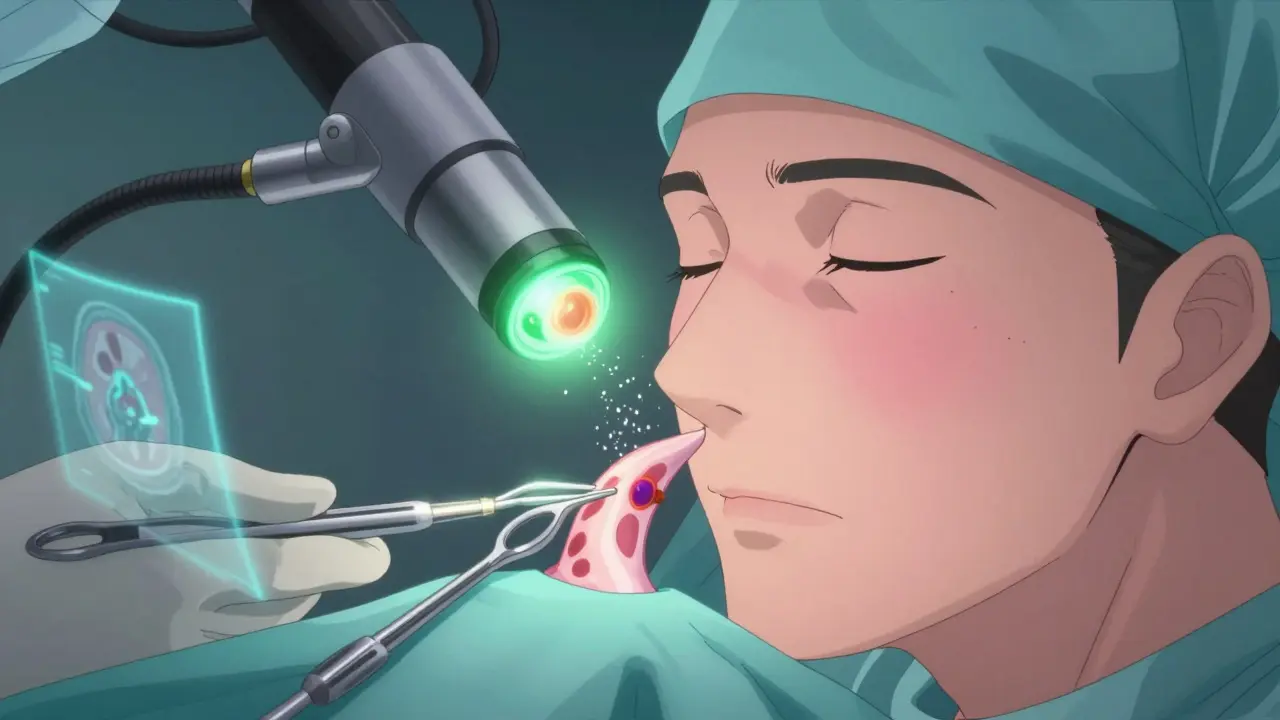
Surgery isn’t the first option. It’s the next step if you’ve tried at least 12 weeks of medical treatment and still have severe symptoms. The gold standard is Functional Endoscopic Sinus Surgery (FESS). During this procedure, an ENT surgeon uses a thin camera and small instruments to remove blockages, open up narrowed sinus passages, and clear out polyps. Success rates are high: 75-90% of patients report lasting improvement.
Recovery is quicker than you might think. Most people go back to work in 7-10 days. There’s no external cutting. Everything is done through the nose.
Another option is balloon sinuplasty. It’s less invasive. A tiny balloon is inflated inside the blocked sinus to widen it. Recovery is faster-3 to 5 days-but long-term results aren’t as strong as FESS. It works best for people with mild blockages and no polyps.
If you have nasal polyps, a polypectomy (removing the polyps) is often done during FESS. But here’s the reality: even after surgery, polyps come back in 40-50% of cases within 18 months if you don’t keep using your steroid spray. Surgery fixes the structure, but you still need the medication to keep inflammation down.
For those with a deviated septum, a septoplasty can be done at the same time. It improves airflow and helps other treatments work better. About 65-75% of patients report major improvement after this combined approach.
Lifestyle Changes That Actually Help
Medication and surgery aren’t the whole story. Daily habits make a big difference.
- Use a humidifier in dry weather. Dry air irritates your sinuses. In places like Sydney, where winter air can get dry, a humidifier in your bedroom cuts symptoms for about 40% of users.
- Avoid smoke, strong perfumes, and air pollution. If you can’t avoid them, wear a mask.
- Stay hydrated. Water keeps mucus thin and easier to drain.
- Wash your pillowcases weekly. Dust mites are a major trigger.
- If you have allergies, try to identify your triggers. Allergy testing can help you avoid what’s making things worse.
What Happens If You Ignore It?
Most people with chronic sinusitis don’t develop serious complications. But untreated inflammation can lead to deeper problems. In less than 0.5% of cases, the infection can spread to the eyes, bones, or even the brain. That’s rare-but it’s why persistent symptoms need attention.
More commonly, it just wears you down. You’re tired. You can’t sleep. You lose your sense of smell and taste. You miss work. You feel like you’re always fighting a cold. That’s why managing it isn’t optional-it’s about your quality of life.
What’s Next? The Future of Treatment
Research is moving fast. Scientists are looking at the sinus microbiome-the bacteria that live in your nose. Early studies suggest certain probiotics might reduce inflammation. Clinical trials are underway to see if adding them to your routine helps.
For people with Samter’s triad, aspirin desensitization is becoming more common. It involves slowly increasing doses of aspirin under medical supervision. About 70-80% of those who complete the process see major improvement in polyps and breathing.
By 2027, experts predict biologics will treat 25-30% of severe chronic sinusitis cases. That means fewer surgeries and better outcomes for people who’ve struggled for years.
Final Thoughts: It’s Manageable
Chronic sinusitis isn’t a death sentence. It’s not something you just have to live with. But it does require patience. You can’t fix it with one pill or one surgery. It’s a long-term plan: saline rinses, steroid sprays, avoiding triggers, and sometimes biologics or surgery. The key is working with your doctor to figure out which subtype you have-and sticking with the treatment that fits.
If you’ve been told it’s just allergies or a bad cold, and nothing’s helped, it’s time to ask for a nasal endoscopy or CT scan. You don’t have to keep breathing through your mouth. You don’t have to lose your sense of smell. There’s a path forward. You just need the right plan.
Is chronic sinusitis caused by bacteria?
No, not usually. While acute sinusitis can be bacterial, chronic sinusitis is mostly caused by inflammation, allergies, nasal polyps, or structural issues. Antibiotics rarely help unless there’s a clear, active bacterial infection-and even then, it’s usually just a temporary flare-up.
How long does it take for nasal steroid sprays to work?
It typically takes 4 to 8 weeks of daily use to see real improvement. Some people feel a little better after 2 weeks, but full benefits take longer. Stopping early is the #1 reason people think the spray didn’t work.
Can nasal polyps come back after surgery?
Yes. In 40-50% of cases, polyps return within 18 months if you don’t continue using a steroid nasal spray. Surgery removes them, but it doesn’t stop the inflammation that causes them. Ongoing medical management is critical.
Is sinus surgery risky?
Functional Endoscopic Sinus Surgery (FESS) is very safe when done by an experienced ENT. It’s done through the nose, so there are no external cuts. Serious complications like bleeding or eye damage occur in less than 1% of cases. Most people return to normal activities within a week.
What’s the difference between FESS and balloon sinuplasty?
FESS removes tissue and opens blocked sinuses completely. Balloon sinuplasty inflates a tiny balloon to widen the passage without removing tissue. FESS has higher long-term success (75-90%) and works better for polyps or severe blockages. Balloon sinuplasty has faster recovery (3-5 days) but lower long-term effectiveness (70-80%) and isn’t ideal for complex cases.
Do I need a CT scan to diagnose chronic sinusitis?
Not always, but it’s often needed. If your symptoms are persistent and don’t respond to treatment, a CT scan helps doctors see if you have polyps, structural problems, or thickened sinus lining. It’s not for diagnosing infection-it’s for understanding the anatomy behind your symptoms.


15 Comments
Ted Conerly
9 January, 2026Saline rinses changed my life. I was skeptical at first, but after two weeks of daily use, I could actually breathe through my nose again. No more midnight coughing fits or waking up with a dry throat. It’s not glamorous, but it works.
Christine Milne
11 January, 2026It is entirely unacceptable that the medical establishment continues to promote unproven, non-pharmaceutical interventions such as nasal irrigation as primary therapy. The empirical evidence for saline irrigation is statistically insignificant, and the reliance on such methods reflects a dangerous decline in evidence-based medicine.
Bradford Beardall
11 January, 2026Really appreciate this breakdown. I’m from India and we’ve got a ton of people dealing with this, especially in cities with high pollution. My uncle had polyps and tried everything until he started using a humidifier and steroid spray. He’s been symptom-free for two years now. Culture doesn’t matter-biology does.
McCarthy Halverson
13 January, 2026Saline works. Steroid spray takes time. Don’t quit early. Polyps come back without maintenance. Surgery helps but isn’t magic. Stick with it.
Michael Marchio
13 January, 2026Let me tell you something about the pharmaceutical industry’s quiet agenda. They don’t want you to know that chronic sinusitis is often caused by mold exposure in modern buildings, especially in air-conditioned offices and homes. The real solution isn’t sprays or surgery-it’s environmental remediation. But why would Big Pharma promote that when they profit from biologics and nasal devices? The data is suppressed. Look at the funding sources behind those ‘clinical trials.’
Jake Kelly
13 January, 2026This is the kind of post that gives hope. I’ve been dealing with this for six years and felt like no one understood. Just knowing there’s a real path forward makes a difference. Thanks for laying it out so clearly.
Ashlee Montgomery
15 January, 2026It’s funny how we treat the body like a machine you fix with tools. But inflammation isn’t a glitch-it’s a signal. Maybe the real question isn’t how to suppress it, but why it’s happening at all. What’s your body trying to tell you? The answer might be in your diet, your stress, your sleep-not just your nasal spray.
neeraj maor
16 January, 2026Biologics? They’re just another way to control the population. The FDA approves these drugs because they’re expensive and require lifelong use. The real cure? Avoiding EMF radiation from 5G towers and fluoride in water. That’s what’s triggering the immune chaos. No one talks about it because the corporations own the labs.
Ritwik Bose
17 January, 2026Thank you for sharing such a thoughtful and well-researched overview 🙏. In India, many people rely on Ayurvedic steam inhalation and turmeric nasal drops. While not a replacement for modern medicine, they can be supportive. I hope more integrative approaches gain recognition. Health is holistic.
Paul Bear
17 January, 2026It is imperative to clarify that the term ‘chronic rhinosinusitis’ is not synonymous with ‘allergic rhinitis’-a common conflation among non-specialists. The pathophysiological distinction is critical: the former is a mucosal inflammatory disorder with neutrophilic or eosinophilic infiltration, whereas the latter is IgE-mediated. Misdiagnosis leads to inappropriate therapeutic sequencing. Furthermore, the use of ‘steroid spray’ without specifying the molecular class (e.g., fluticasone propionate vs. mometasone furoate) is clinically imprecise and potentially misleading.
lisa Bajram
19 January, 2026OMG I was SO done with this until I found out about the humidifier trick!! I live in Arizona and my sinuses were screaming every winter. Got a little $20 humidifier for my bedroom and now I actually sleep without waking up with my nose stuffed like a pillow. Also, washing pillowcases weekly? Game changer. I used to think it was just ‘allergies’-turns out it was dust mites throwing a rave on my pillow. 🙃
Jaqueline santos bau
19 January, 2026I’ve been through FESS twice and now I’m on Dupixent and I swear I’ve never felt this good in my life-but my husband says I’m obsessed. I talk about my nasal spray like it’s my baby. I cry when I run out. I have spreadsheets tracking my mucus color. Is this normal? Am I the only one who treats this like a full-time job? I just want to smell coffee again without crying.
Kunal Majumder
20 January, 2026My dad had this for 15 years. Tried everything. Then he started doing saline rinses every morning and stopped drinking cold soda. That’s it. No surgery. No biologics. Just clean water and patience. Sometimes the simplest things work the best.
Aurora Memo
20 January, 2026Thank you for writing this. It’s easy to feel alone with this condition. You’re not just managing symptoms-you’re reclaiming your life. And that’s worth every drop of saline and every day of waiting for the spray to work.
Ted Conerly
21 January, 2026Re: the comment about mold and 5G-there’s no credible evidence linking those to chronic sinusitis. The real environmental triggers are well-documented: PM2.5, cigarette smoke, dry air. Stick to the science.