Cyclosporine Safety Checker
Your Cyclosporine Levels
Kidney Function
Please check your values
Enter values to see safety status
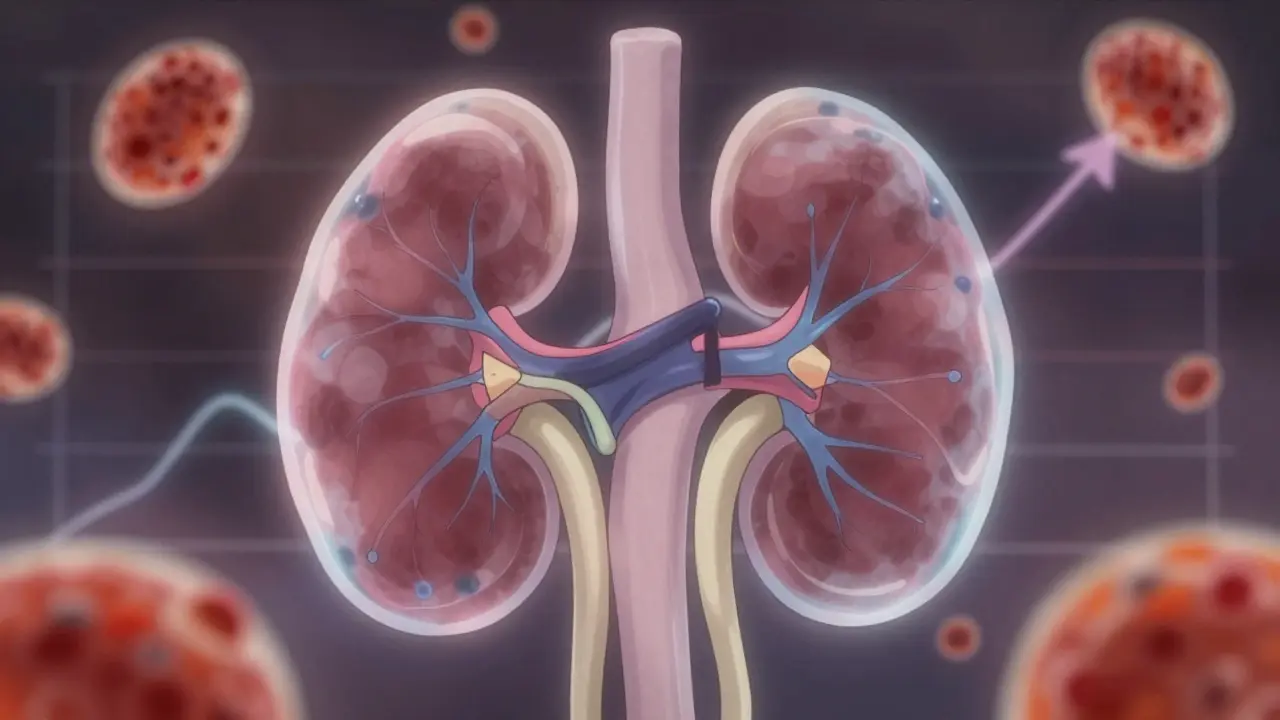
Why Cyclosporine Can Hurt Your Kidneys
When you take cyclosporine after a transplant, it’s doing its job: stopping your immune system from attacking the new organ. But it’s also quietly putting pressure on your kidneys. About 1 in 3 people on this drug will show signs of kidney damage within the first year. It’s not always obvious-no pain, no fever, no warning signs. Just a slow rise in creatinine, a subtle drop in urine output, or a blood pressure reading that won’t budge. That’s why monitoring isn’t optional. It’s the difference between keeping your transplant alive and losing it.
What Makes Cyclosporine So Dangerous for Kidneys
Cyclosporine doesn’t just kill immune cells. It tightens the blood vessels inside your kidneys, reducing blood flow. This isn’t a side effect-it’s the drug’s main mechanism. Over time, this causes scarring in the tiny arteries, thickening of the walls, and damage to the tubules where waste gets filtered. Think of it like squeezing a garden hose too hard: the water still flows, but not as well, and the hose eventually wears out. The higher the dose and the longer you’re on it, the worse the damage gets. And here’s the catch: the same blood levels that prevent rejection can also start killing kidney cells. That’s why staying within the narrow window is everything.
How Doctors Track Cyclosporine Levels
It’s not enough to guess the dose. You need to know exactly how much drug is in your blood. There are two main ways this is measured: trough levels (C0) and peak levels (C2). Trough levels are drawn right before your next dose, when the drug is at its lowest. This has been the standard for decades. But newer research shows that measuring the level two hours after you take your pill-called C2-gives a much clearer picture of how much drug your body is actually absorbing. Studies show C2 monitoring cuts rejection rates by nearly 20% and reduces kidney damage by over 20%. The reason? It catches people who metabolize the drug too fast or too slow, something trough levels often miss.
Lab tests used to rely on immunoassays-fast and cheap, but often wrong. These tests can’t tell the difference between cyclosporine and its metabolites, which can inflate readings by up to 15%. That means a doctor might think you’re safe when you’re actually overdosing. Today, most top transplant centers use LC-MS/MS (liquid chromatography-tandem mass spectrometry). It’s accurate to 99.2%, detects levels as low as 5 ng/mL, and doesn’t get fooled by metabolites. If your lab still uses older methods, ask if they’ve upgraded. Your kidneys will thank you.
Target Blood Levels by Time After Transplant
There’s no one-size-fits-all number. Your target changes over time. Here’s what current guidelines recommend:
- First week after transplant: 200-400 ng/mL
- Week 2 to 6 months: 125-275 ng/mL
- 7 to 12 months: 100-150 ng/mL
- After 1 year: 75-160 ng/mL
For heart and liver transplants, the ranges are similar. But if you’re a CYP3A5 extensive metabolizer (about 10-15% of people), your body clears the drug faster. You might need 30-40% more to reach the same level. Genetic testing is now available-ask your doctor if you’ve been tested. If not, it’s worth considering.
What Kidney Function Tests to Watch
Cyclosporine levels alone don’t tell the whole story. You need to track how your kidneys are responding. Here’s what your care team should check regularly:
- Serum creatinine: Keep it under 1.5 mg/dL. A steady rise over weeks, even if still below 1.5, is a red flag.
- BUN-to-creatinine ratio: Should be under 20:1. Higher ratios suggest reduced kidney blood flow.
- Blood pressure: Must stay under 130/80 mmHg. Cyclosporine causes high blood pressure in half of users. Uncontrolled BP speeds up kidney damage.
- Magnesium: Levels below 1.7 mg/dL are common and linked to worse kidney outcomes. Many patients need daily supplements.
- Urine output: Less than 0.5 mL/kg/hour over 24 hours means your kidneys are struggling.
Don’t wait for your next appointment if your legs swell, you’re urinating less, or your blood pressure spikes. Call your transplant team immediately.
Drug Interactions That Can Crash Your Kidneys
Many common medications change how your body handles cyclosporine. A simple antibiotic or antifungal can push your levels into toxic territory.
- Never combine with ketoconazole, itraconazole, or clarithromycin. These can spike cyclosporine levels by 30-50%.
- Avoid rifampin, St. John’s wort, or phenytoin. These can drop your levels by 40-60%, raising rejection risk.
- Be careful with NSAIDs. Ibuprofen, naproxen-even over-the-counter ones-can reduce kidney blood flow and worsen damage.
- Antacids with magnesium or aluminum can bind cyclosporine and reduce absorption. Take them at least 2 hours apart.
Always tell every doctor you see-including dentists-that you’re on cyclosporine. A single prescription from someone who doesn’t know your history could be dangerous.
When and How Often to Test
Testing frequency isn’t set in stone-it depends on your stability.
- First month: Twice a week
- Months 2-6: Once a week
- Months 7-12: Every two weeks
- After 1 year: Monthly, or as directed
After any dose change, wait 4-6 weeks before retesting. That’s how long it takes for levels to stabilize. Don’t rush it. Also, always use EDTA tubes (purple top) for blood draws. Serum separator tubes (red or gold top) can give falsely high readings by up to 20% because cyclosporine sticks to the gel. If your lab uses the wrong tube, ask them to switch.
Can the Damage Be Reversed?
Yes-but only if caught early. If your creatinine rises and you reduce your dose quickly, kidney function often improves within 6-12 weeks. Studies show that 70% of patients with early-stage damage recover most of their function after adjusting cyclosporine. But if scarring sets in-visible on biopsy or shown by persistently high creatinine over months-it’s permanent. That’s why waiting is the worst thing you can do. The moment your numbers start creeping up, act. Don’t wait for symptoms. Don’t hope it’ll fix itself. Your transplant depends on your vigilance.
What’s Next for Cyclosporine Monitoring
Researchers are already moving beyond blood draws. Clinical trials are testing AI systems that predict your ideal dose using 17 variables-your weight, age, genetics, diet, even your sleep patterns. Early results show 89.7% accuracy. There are also point-of-care devices in Phase 3 trials that can give you a full cyclosporine reading in under 15 minutes using just a finger prick. These won’t replace labs yet, but they’ll make monitoring less painful and more frequent. In the next five years, we’ll likely see personalized dosing algorithms built right into transplant care apps. But for now, the old rules still hold: know your numbers, know your meds, and never ignore a rising creatinine.
Can I stop taking cyclosporine if my kidney numbers go up?
Never stop cyclosporine without your transplant team’s direction. Stopping suddenly can trigger acute rejection, which may destroy your new organ within days. If your kidney function declines, your doctor will adjust your dose, add another immunosuppressant like mycophenolate, or switch you to tacrolimus-but only after careful evaluation. Self-discontinuation is dangerous and can be life-threatening.
Is cyclosporine still used today, or has it been replaced?
Cyclosporine is still used in about 150,000 transplant patients in the U.S. each year. While newer drugs like tacrolimus are often preferred because they’re less toxic to kidneys, cyclosporine remains vital for patients who can’t tolerate tacrolimus due to neurological side effects, diabetes risk, or cost. It’s also used in autoimmune diseases like severe psoriasis and nephrotic syndrome. It’s not outdated-it’s just used more carefully now.
Why do some labs report different cyclosporine levels than others?
Different testing methods give different results. Immunoassays often overestimate levels by 10-15% because they detect metabolites, not just the active drug. LC-MS/MS is the gold standard and gives the most accurate reading. If you switch labs or hospitals, always ask what method they use. Your target range may need to be adjusted based on the test type. Never compare numbers from different labs without knowing the method.
Can diet or alcohol affect cyclosporine levels?
Yes. Grapefruit juice can increase cyclosporine levels by up to 50% because it blocks enzymes that break down the drug. Alcohol doesn’t directly affect levels, but it stresses the liver and kidneys, making toxicity more likely. Avoid grapefruit entirely. Limit alcohol to one drink a day at most, and only if your doctor says it’s safe. Consistency matters-don’t drink one day and skip the next. Your body needs stable conditions to process the drug properly.
What if I miss a dose of cyclosporine?
If you miss a dose by less than 6 hours, take it as soon as you remember. If it’s more than 6 hours late, skip it and take your next dose at the regular time. Never double up. Missing doses increases rejection risk. But taking two doses close together can cause toxic spikes. Keep a log or use a pill organizer with alarms. If you miss more than one dose in a week, contact your transplant coordinator immediately.
Final Thought: Your Kidneys Are Your Lifeline
Cyclosporine saved your life by giving you a new organ. But it’s also a slow, silent threat to that same organ. The only way to win this balance is through constant, precise monitoring. Know your numbers. Know your meds. Know your body. The best transplant outcomes don’t come from luck-they come from discipline. Stay on top of your labs. Ask questions. Push back if something feels off. Your kidneys can’t speak for themselves. You have to speak for them.

11 Comments
Eliana Botelho
30 January, 2026I get that cyclosporine is necessary but honestly? It feels like we're just trading one problem for another. My cousin went from needing a kidney transplant to needing a second one because of this drug. They told her the levels were 'in range' but her creatinine kept climbing. She ended up on dialysis for six months before they switched her. Why aren't we talking more about alternatives? Like, why is this still first-line when tacrolimus exists? And don't even get me started on how often labs mess up the readings. I swear half the time my results don't even make sense between visits.
Rob Webber
31 January, 2026This entire post is a glorified pharmaceutical ad. Cyclosporine isn't 'saving lives'-it's keeping people alive on a ticking time bomb while drug companies rake in billions. The fact that you need LC-MS/MS to even get a semi-accurate reading means the drug shouldn't be approved in the first place. And don't even mention those 'target ranges'-they're just guesses dressed up as science. I've seen people die because their doctor trusted a flawed immunoassay. This isn't medicine. It's roulette with kidneys.
calanha nevin
2 February, 2026Critical information presented clearly. Trough levels alone are inadequate. C2 monitoring is non-negotiable for stable long-term outcomes. Magnesium supplementation is underutilized and often overlooked. Many patients present with hypomagnesemia and are misdiagnosed as dehydrated. Always check electrolytes before assuming volume status. Also, EDTA tubes are mandatory. Serum separator tubes produce artifactually elevated values due to drug binding to gel. This is not a minor detail-it is a systemic failure in many community labs. Advocate for proper methodology. Your transplant depends on it.
Claire Wiltshire
3 February, 2026Thank you for this comprehensive overview. It's refreshing to see such precise guidance on monitoring protocols. I particularly appreciate the emphasis on C2 levels and the distinction between immunoassays and LC-MS/MS. Many patients are unaware that their lab's method affects their entire treatment trajectory. For those managing cyclosporine long-term, consistency in testing location and methodology is as vital as adherence to dosing. Small deviations compound over time. Please share this with your care team. Knowledge is protection.
Darren Gormley
3 February, 2026This is why I hate modern medicine 🤡 Cyclosporine? More like Cyclo-SCAM. They tell you to avoid grapefruit but not that your coffee might be lowering your levels by 12% because of the roast. Also-did you know the FDA only approved this because a guy in a lab coat said 'it works' in 1983? No long-term studies. No real safety data. Just a bunch of doctors nodding while their pharma reps handed out pens. I'm not saying don't take it. I'm saying you're being used as a test subject. P.S. Your kidneys are not your lifeline. They're your collateral damage.
Sidhanth SY
4 February, 2026I'm a transplant recipient from India and this is exactly what we've been learning here too. The C2 monitoring is becoming more common in our big hospitals now. We had a case where someone's levels looked fine on immunoassay but were actually toxic-switched to LC-MS/MS and the creatinine dropped in two weeks. Also, magnesium supplements are a game changer. I started taking 400mg daily and my BP stabilized. It's not magic, but it's simple. And yes, grapefruit juice is a hard no. I stopped drinking it cold turkey after my nurse showed me the data.
Beth Cooper
5 February, 2026Wait. Did you know cyclosporine was originally developed as an antifungal? And then they found out it suppressed immunity? That’s not science-that’s accidental. And now we’re giving it to people for decades? I bet the FDA never tested it with kombucha or turmeric. And what about the 20% error rate with serum tubes? That’s not a mistake. That’s negligence. Someone’s hiding something. Why aren’t there class action lawsuits? Why are we still using this? This feels like a controlled experiment. And I’m not the only one who thinks so.
Donna Fleetwood
7 February, 2026I know this stuff is heavy but you’re doing amazing just by reading this and asking questions. I was on cyclosporine for 8 years after my liver transplant. I thought I was fine until my creatinine hit 1.7. I panicked. But I called my team immediately, we dropped the dose, added mycophenolate, and within 3 months my kidneys bounced back. You’re not alone. Small steps matter. You’re not failing if you need to adjust. You’re surviving. Keep going. You’ve got this.
Bobbi Van Riet
7 February, 2026I’ve been on cyclosporine for 11 years and I’ve learned so much the hard way. The thing no one tells you is that your body changes. What worked at 6 months doesn’t work at 5 years. I had to switch from twice-daily to three times-daily dosing because my metabolism shifted. Also, I started tracking my urine output with a measuring cup-it sounds weird but it saved me. One day I noticed I was only peeing 400mL total and called my nurse. Turned out my level was creeping up. They lowered my dose before it got worse. Don’t wait for symptoms. Track the numbers. Even the small ones. And if your doctor rolls their eyes at your questions? Find a new one. You deserve better.
Lily Steele
7 February, 2026Just wanted to say thank you for this. I’ve been scared to ask my doctor about C2 testing because I thought I’d sound like a know-it-all. Turns out she’d been meaning to bring it up too. We switched labs and now my numbers make sense. Also started taking magnesium. My legs aren’t swollen anymore. Small changes. Big difference. You’re not crazy for paying attention. You’re the only one who knows your body best.
Carolyn Whitehead
8 February, 2026I’m still learning but this helped me understand why my creatinine keeps going up even though I take my pills. I didn’t realize grapefruit juice was that bad. I’ll stop it. And I’ll ask about the tube type next time I get blood drawn. Thanks for not making me feel dumb for not knowing this stuff.