When a life-saving drug runs out, who gets it? This isn’t science fiction. In 2023, hospitals across the U.S. faced severe shortages of carboplatin and cisplatin-two key chemotherapy drugs used to treat ovarian, lung, and testicular cancers. Some patients waited weeks for treatment. Others were told their dose would be cut in half. A few didn’t get it at all. Behind these decisions were teams of doctors, pharmacists, and ethicists trying to do the right thing under impossible conditions.
Why Medication Rationing Happens
Drug shortages aren’t new, but they’ve gotten worse. In 2005, there were 61 reported shortages in the U.S. By 2023, that number jumped to 319. The biggest culprits? Generic injectable drugs-especially cancer meds, antibiotics, and anesthetics. Three companies control 80% of the supply for these critical drugs. If one factory shuts down for quality issues, or if a raw material gets delayed overseas, the whole system stumbles. The FDA requires manufacturers to give a six-month heads-up before a shortage hits. But only 68% actually do. That leaves hospitals scrambling. In community clinics, 87% reported severe shortages of key chemo drugs. Even big hospitals weren’t safe-63% struggled to keep up. When supply drops below demand, doctors can’t just prescribe what’s needed. They have to choose. And that’s where ethics kicks in.What Ethical Rationing Actually Looks Like
Ethical rationing isn’t about picking patients based on age, income, or who screams loudest. It’s about using clear, fair rules so no one’s left to guess who gets treated. The most trusted framework comes from ethicists Daniel and Sabin. Their model has four rules:- Publicity: Everyone knows how decisions are made.
- Relevance: Decisions are based on medical facts-not gut feelings.
- Appeals: Patients or families can challenge a decision.
- Enforcement: Someone checks that the rules are followed.
What Happens When There’s No System
Too often, there’s no committee. No rules. Just whoever’s on call deciding who gets the last vial. A 2022 study found 52% of rationing decisions were made by individual clinicians-no review, no discussion. That leads to chaos. One nurse in Texas told a reporter she had to give her last dose to a 28-year-old because the 68-year-old “had already had a good life.” That’s not ethics. That’s grief talking. Bedside rationing also burns out staff. Clinicians who make these calls alone are 27% more likely to report burnout. And patients? Only 36% are told they’re being rationed. Imagine being told your treatment is delayed-without knowing why. That’s not just unfair. It’s traumatic. Hospitals with formal committees report 41% less moral distress among staff. They also see fewer disparities. Patients of color, low-income patients, and those without strong advocates are far more likely to be left out when decisions are made informally.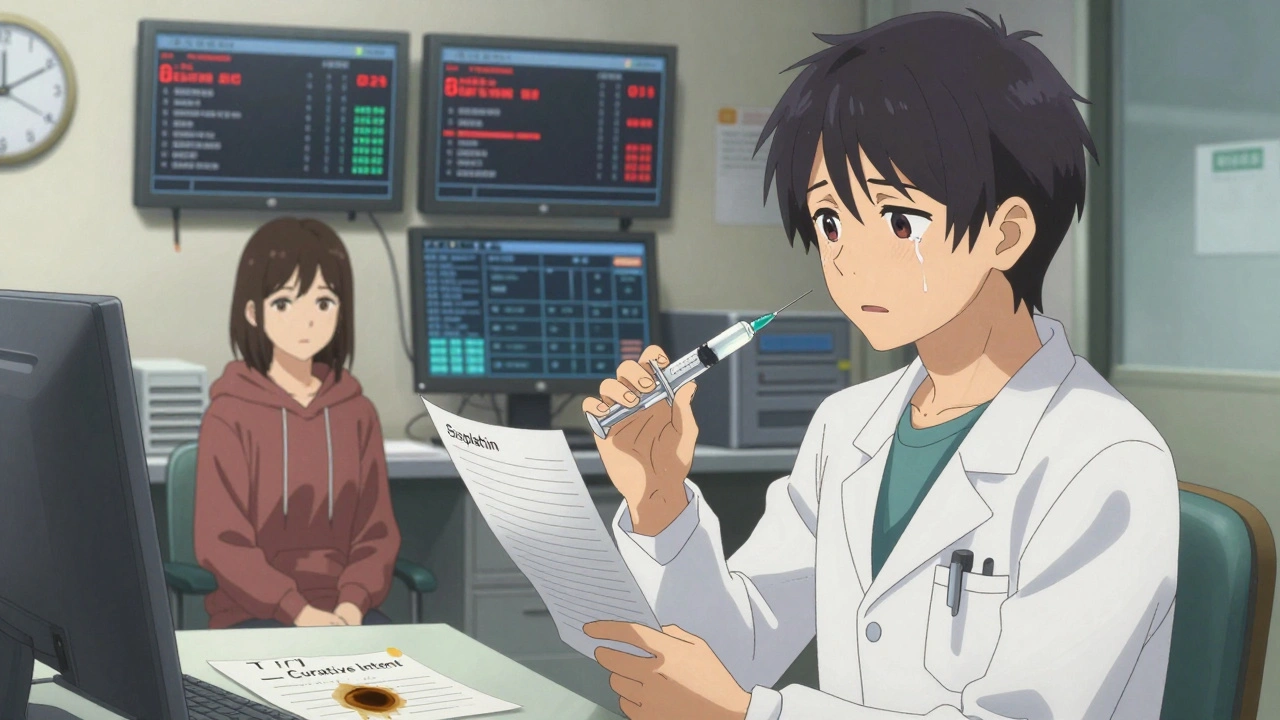
How Hospitals Are Trying to Fix This
Some places are getting better. Minnesota’s Department of Health released a detailed guide in April 2023 for carboplatin and cisplatin shortages. It didn’t just say “be fair.” It said:- Tier 1: Curative intent, no alternative drug available
- Tier 2: Palliative intent, but high chance of symptom control
- Tier 3: Low benefit, high risk
The Big Gaps
Even with good frameworks, big problems remain. Rural hospitals? 68% have no formal rationing plan. They don’t have ethicists on staff. No pharmacy teams. Sometimes, they don’t even have a pharmacist on-site. And equity? Most protocols don’t even measure it. A 2021 report found 78% of rationing guidelines ignore race, income, or language barriers. That means patients who already face healthcare gaps get pushed further behind. Doctors also say they’re not trained for this. In a 2023 survey, 89% of pharmacists said the biggest problem was inconsistent rules across departments. One unit hoards drugs. Another gives them away too fast. No one’s watching.
What’s Next?
The FDA is building an AI-powered early warning system to predict shortages before they happen. It’s supposed to cut shortage duration by 30% by 2025. That’s promising. The National Academy of Medicine is working on national standards for ethical allocation. Draft criteria are due in early 2024. They’ll likely include metrics for fairness, survival benefit, and equity. And in January 2024, pilot programs launched in 15 states to certify hospital rationing committees. Think of it like CPR certification-but for ethical drug allocation. Hospitals that pass get a seal of approval.What You Can Do
If you or someone you love is facing a shortage:- Ask: Is there a formal committee making these decisions?
- Ask: Can I see the criteria used to prioritize patients?
- Ask: Was I told why my treatment changed?
- Ask: Are there alternatives? Clinical trials?
Final Thought
Rationing isn’t about who deserves to live. It’s about who gets treated when there’s not enough to go around. And if we don’t make the rules clear, fair, and public-we’re not just failing patients. We’re failing the people who care for them.Every doctor wants to help. But when they’re forced to play god without a manual, everyone loses. The solution isn’t more drugs-though we need those too. It’s better systems. Clear rules. And the courage to talk about hard choices before it’s too late.
Is medication rationing legal?
Yes, but only when done ethically and transparently. In the U.S., there’s no federal law mandating rationing, but courts have upheld hospital policies that follow clear, evidence-based guidelines. Rationing becomes illegal if it’s based on discrimination, bias, or secrecy. The key is having documented criteria, a review process, and patient notification.
Can I request a specific drug if it’s on shortage?
You can ask, but you can’t demand it. Hospitals must follow their allocation protocols. If you’re denied a drug, ask for the written policy, the reason for denial, and whether an appeal is possible. Some hospitals have patient advocates who can help navigate this process.
Why aren’t more hospitals using ethics committees?
Cost, time, and resistance. Setting up a committee takes training, staff time, and ongoing meetings. Many hospitals don’t have enough ethicists or pharmacists to staff them. Some doctors resist because they fear losing control over patient care. But data shows hospitals with committees have less burnout and fewer lawsuits.
Are there alternatives when a drug is unavailable?
Yes, but not always. For some cancer drugs like cisplatin, there are no equally effective substitutes. In those cases, doctors may use carboplatin instead, though it’s less effective for some tumors. For antibiotics, alternatives exist but may have more side effects. Always ask your care team: Is there another option? What are the trade-offs?
How can I find out if a drug I take is in short supply?
Check the FDA’s Drug Shortages page, which is updated weekly. Your pharmacist can also alert you. For cancer drugs, ASCO’s website has real-time alerts. If your medication is listed, talk to your doctor early-don’t wait until your refill runs out.

9 Comments
Inna Borovik
7 December, 2025Let’s be real-this isn’t about ethics. It’s about who has the best insurance, the loudest advocate, or the most connected doctor. I’ve seen it. A patient with a private oncologist got their full dose while someone on Medicaid got half. The committee? A PowerPoint slide they never showed patients. Transparency is a buzzword until it’s your life on the line.
And don’t get me started on ‘dose optimization.’ That’s just corporate-speak for ‘we’re stretching the last vial until it snaps.’ It’s not innovation. It’s triage by spreadsheet.
Rashmi Gupta
7 December, 2025Everyone’s talking about ‘fairness’ like it’s a math problem. But what’s fair about a 72-year-old getting chemo because ‘they’ve lived enough’? That’s not ethics-that’s eugenics wrapped in a hospital badge. And the FDA’s AI system? Please. It’ll just learn to prioritize white, insured patients because that’s what the data says. History doesn’t lie.
Andrew Frazier
7 December, 2025USA got the best meds in the world and we’re whining about rationing? In India they make these drugs for pennies and still get them to people. Why? Because they don’t have 12 layers of bureaucracy and lawyers making everything a lawsuit waiting to happen. Just let the doctors decide. If you’re sick, you get it. If you’re not? Too bad. Stop overthinking and fix the supply chain.
Also, who the hell is this ‘ASCO’? Sounds like a yoga studio.
Mayur Panchamia
8 December, 2025I am not surprised. American healthcare is a circus. We pay $10,000 for a pill that costs $2 to make-then we cry when it runs out?!!! The real problem? Pharma monopolies. Three companies. Three. And they sit in their air-conditioned offices laughing while old people die waiting for cisplatin. We need nationalization. Not committees. Not ‘guidelines.’ Just make it public. Make it free. Or we will burn it down. 🔥
Nava Jothy
9 December, 2025My heart is breaking. 😢
Imagine being told your child’s treatment is delayed because someone else ‘has a better chance.’ That’s not medicine-that’s soul-crushing moral calculus. And who gets to decide? A committee of strangers who’ve never held a dying patient’s hand? I’ve sat in those chairs. I’ve heard the silence after the doctor says, ‘We don’t have enough.’
They talk about ‘transparency’ like it’s a Band-Aid. But no one talks about the trauma. The guilt. The nightmares. The nurses crying in the supply closet. We need more than protocols-we need humanity.
And yes, I’m crying right now typing this. 💔
brenda olvera
10 December, 2025this is so important and i'm so glad someone is finally talking about it
we need to stop pretending this is just a medical issue
it's a moral one
and if we can fix this we can fix so much more
keep pushing for change
you're not alone
Saketh Sai Rachapudi
11 December, 2025India makes 80% of the world's generic drugs and still we dont have this problem. Why? Because we dont have greedy pharma execs running things. Here in US its all profit. If you dont have money you die. Simple. No committee can fix that. Only revolution can. And its coming. Just wait.
Also why are we letting foreigners decide our healthcare? The FDA? ASCO? Who elected them?
Gwyneth Agnes
13 December, 2025No one talks about the nurses. They’re the ones holding the vials. They know who’s waiting. They see the tears. They’re the ones who get blamed when someone dies. No committee. No training. Just silence.
Katie O'Connell
14 December, 2025While the structural inefficiencies of pharmaceutical supply chains are undeniably problematic, the ethical frameworks underpinning allocation protocols-particularly those derived from the Daniel and Sabin model-represent a necessary, if imperfect, attempt to operationalize distributive justice in resource-constrained environments. The absence of standardized, multi-disciplinary oversight mechanisms in rural institutions constitutes a systemic failure of governance, not merely of logistics. One must, however, caution against conflating procedural fairness with equitable outcomes, particularly when sociodemographic variables remain unquantified in allocation algorithms. The proposed AI-based predictive system, while technologically intriguing, risks reinforcing latent biases unless trained on demographically stratified, real-time clinical datasets. Further, the normalization of ‘dose optimization’ as a palliative strategy may inadvertently normalize therapeutic under-treatment, particularly among marginalized populations who lack the institutional capital to advocate for alternative regimens. Ethical rationing, therefore, must transcend proceduralism and embed equity as a primary, measurable outcome-not a secondary consideration.