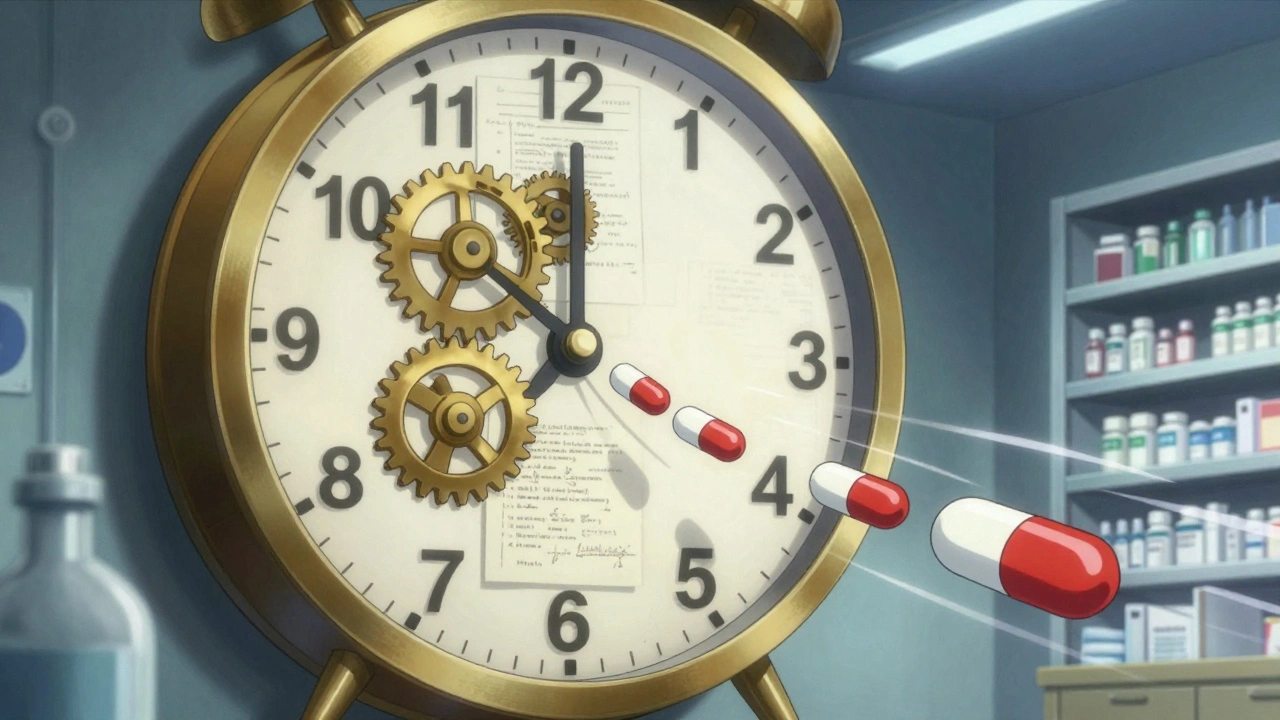
Patent Cliff: What Happens When Drug Monopolies End and Prices Drop
When a drug’s patent cliff, the moment when a drug’s exclusive manufacturing rights expire, allowing competitors to sell identical versions. Also known as patent expiration, it’s when prices for once-expensive medications can drop by 80% or more overnight. This isn’t just a business event—it’s a health event. Every year, dozens of top-selling drugs hit this wall, and if you take any of them, your wallet and your doctor’s prescribing habits will change.
The generic drugs, chemically identical versions of brand-name medicines sold after patent expiration that follow the patent cliff aren’t cheaper because they’re lower quality—they’re cheaper because no one has to pay for R&D, marketing, or flashy ads anymore. The FDA requires them to work the same way, in the same dose, and with the same safety profile. But here’s the catch: not every pharmacy stocks them right away, and not every doctor automatically switches you over. That’s why so many people keep paying full price long after generics are available.
The pharmaceutical patents, legal protections that let companies sell a drug without competition for 20 years are designed to reward innovation, but they also create artificial scarcity. When that protection ends, the market floods with options. You might see your statin, your blood pressure pill, or your diabetes med suddenly cost $5 instead of $300. But the transition isn’t always smooth. Some patients get confused. Some insurers delay coverage. Some pharmacies don’t even tell you the cheaper version exists.
And then there’s the brand-name drugs, original medications sold under a proprietary name before generics enter the market companies. They don’t just sit back. They often tweak the formula just enough to get a new patent—change the pill shape, add a slow-release coating, or bundle it with another drug. These tricks delay the patent cliff, sometimes for years. That’s why you might still be paying high prices even when the original patent expired.
What you’ll find in these articles isn’t theory. It’s real-world stuff: how to ask for generics without sounding like you’re cutting corners, why some people still get brand-name drugs even when generics are cheaper, how insurance tricks keep you paying more, and what happens when a blockbuster drug like Lipitor or Humira finally goes generic. You’ll see how patients saved hundreds—or even thousands—by switching at the right time. You’ll learn what to say to your pharmacist when they try to give you the expensive version. And you’ll understand why some drugs stay pricey long after their patents should’ve expired.
This isn’t about pharmaceutical companies being good or bad. It’s about knowing when the rules change—and how to use that to your advantage. If you’re on any long-term medication, the patent cliff is coming for it. The question is: will you be ready?