If you have type 2 diabetes, your bones might be at risk-even if you feel fine. Many people assume diabetes is just about blood sugar, but it quietly weakens your skeleton over time. You could be walking around with low bone density and not know it until you fall and break something. The good news? You can protect your bones. It’s not about taking extra supplements. It’s about making smart, daily choices that work with your body, not against it.
Why Type 2 Diabetes Weakens Bones
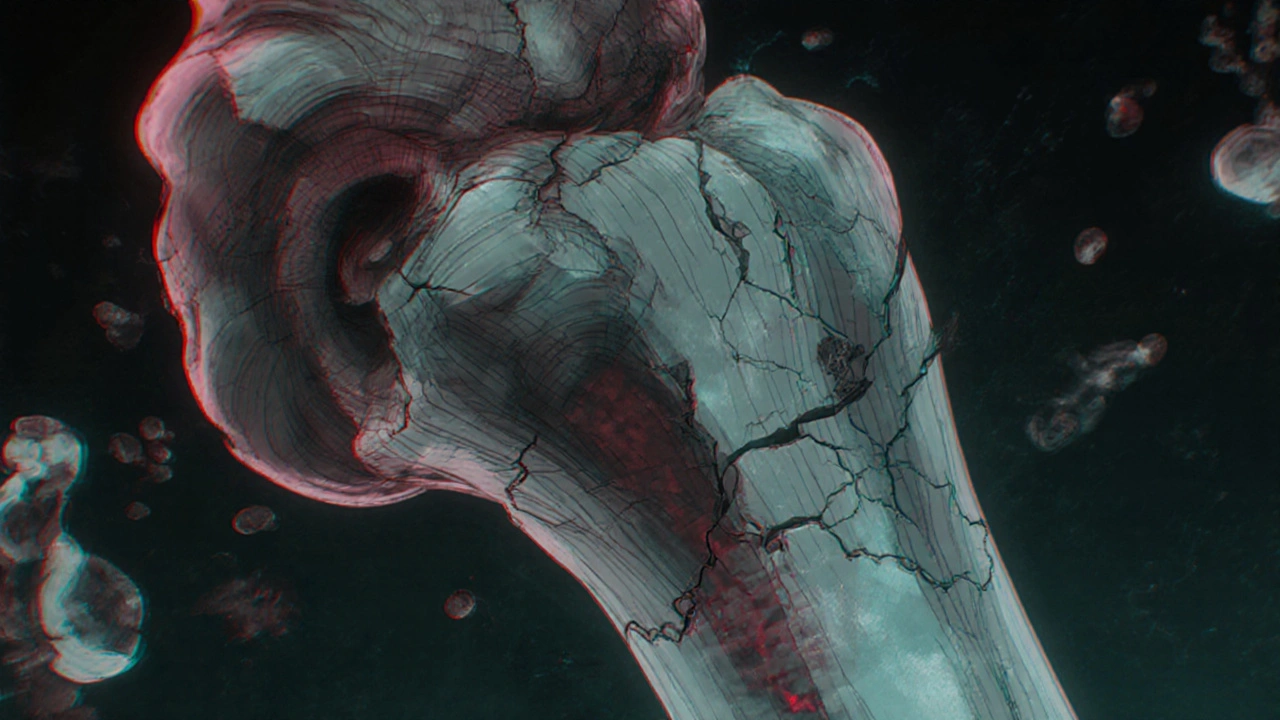
High blood sugar doesn’t just damage nerves and kidneys. It also interferes with how your bones rebuild themselves. Your bones are always breaking down old tissue and building new, strong material. This process is called remodeling. In type 2 diabetes, high glucose levels slow down bone formation and speed up bone loss. Studies show people with type 2 diabetes have a 50% higher risk of breaking a hip than those without diabetes, even when their bone density scans look normal.
Insulin plays a big role here. It’s not just a blood sugar regulator-it’s also a bone-building hormone. When your body doesn’t use insulin well (insulin resistance), your bones don’t get the signal to grow strong. At the same time, chronic inflammation from diabetes damages bone cells. And if you’re taking certain diabetes meds like thiazolidinediones (pioglitazone, rosiglitazone), you might be losing bone mass faster. These drugs were designed to improve insulin sensitivity, but they accidentally trigger fat cells to replace bone cells in your marrow.
Low Bone Density Isn’t Always Seen on Scans
Here’s the tricky part: your DXA scan (the standard bone density test) might say your bones are fine. But that doesn’t mean they’re strong. People with type 2 diabetes often have normal or even high bone mineral density on scans, yet still break bones more easily. Why? Because their bone quality is poor. The structure is brittle, the collagen is damaged, and the microarchitecture is fragile. Think of it like concrete with weak rebar inside-it looks solid, but it cracks under pressure.
That’s why doctors now look beyond just bone density. They check for other signs: a history of fractures after minor falls, slow-healing wounds, or nerve damage (neuropathy) that affects balance. If you’ve broken a bone from a fall from standing height or less, that’s a red flag-even if your scan looks normal.
What You Can Do: 5 Proven Ways to Strengthen Your Bones
Strong bones don’t come from pills alone. They come from daily habits that support your whole body. Here’s what actually works:
- Move your body every day-not just walking, but weight-bearing and resistance exercise. Walking helps, but lifting weights, doing squats, or even climbing stairs builds bone. A 2023 study in Diabetologia found that people with type 2 diabetes who did strength training twice a week improved their bone density by 3.5% in just six months. You don’t need heavy weights. Start with bodyweight exercises: wall push-ups, chair squats, step-ups. Do 10 reps, three times a week.
- Get enough vitamin D and calcium-but don’t overdo it. Most adults need 1,000-1,200 mg of calcium daily and 600-800 IU of vitamin D. Food sources are better than pills. Try yogurt, canned sardines with bones, kale, broccoli, and fortified plant milks. If you’re not getting sun (especially in winter), a vitamin D supplement is worth considering. Ask your doctor to check your levels-many diabetics are deficient.
- Stop smoking and limit alcohol-both wreck bone health. Smoking cuts blood flow to bones and slows healing. Alcohol interferes with calcium absorption and increases fall risk. If you smoke, quit. If you drink, keep it to one drink a day or less.
- Manage your blood sugar tightly-this isn’t just for your heart or kidneys. Stable blood sugar means less inflammation, better insulin function, and stronger bones. A1c levels above 7% are linked to faster bone loss. Aim for consistent numbers, not just occasional spikes.
- Make your home fall-proof-because even strong bones can break if you trip. Remove loose rugs, install grab bars in the bathroom, add nightlights, and wear shoes with good grip. If you have neuropathy in your feet, you might not feel a stumble coming. Prevention matters more than treatment.
Medications That Help-or Hurt
Not all diabetes meds affect bones the same way. Metformin, the first-line drug, might actually protect bone. Some studies suggest it helps bone cells survive and grow. GLP-1 agonists like semaglutide (Ozempic) and liraglutide (Victoza) are also linked to better bone outcomes, possibly because they help with weight loss and reduce inflammation.
On the flip side, thiazolidinediones (Actos, Avandia) should be avoided if you have low bone density or a history of fractures. SGLT2 inhibitors (Jardiance, Farxiga) are newer and still being studied, but early data shows they might slightly increase fracture risk in older adults, especially women. Always talk to your doctor before switching meds-not because you need to stop them, but because you need to know the trade-offs.
If your bones are already weak, your doctor might recommend a bone-strengthening drug like bisphosphonates (alendronate, risedronate). These are common for osteoporosis, but they’re not always right for diabetics. They work best when bone turnover is high. In type 2 diabetes, turnover is often low, so these drugs might not help as much. Your doctor may order a blood test called NTx or CTx to measure bone breakdown before deciding.
What to Ask Your Doctor
Don’t wait for symptoms. Ask these questions at your next check-up:
- “Should I get a bone density scan, even if I haven’t broken a bone?”
- “Could any of my medications be affecting my bones?”
- “What’s my current vitamin D level, and do I need a supplement?”
- “Do I have signs of neuropathy that could increase my fall risk?”
- “Can you refer me to a physiotherapist who understands diabetes and bone health?”
Most doctors don’t screen for bone health in type 2 diabetes unless you’re over 65 or have had a fracture. But if you’re over 50 and have diabetes, you’re at higher risk. Push for a scan if you’re concerned. It’s a simple, painless test that takes 10 minutes.

Real-Life Example: Maria’s Story
Maria, 62, from Sydney, was diagnosed with type 2 diabetes five years ago. She walked daily and ate “healthy,” but she never thought about her bones. Last winter, she slipped on wet pavement and broke her wrist. Her DXA scan showed normal density, but her doctor noticed her bones looked fragile under the microscope. She started doing resistance training twice a week, added vitamin D, and switched from pioglitazone to metformin. Six months later, her balance improved, her blood sugar stabilized, and her next scan showed a 4% increase in bone strength. She didn’t just heal-she rebuilt.
What You Should Avoid
Don’t fall for quick fixes. Bone health isn’t about drinking milk or popping calcium pills without movement. You can’t out-supplement a sedentary lifestyle. Avoid these myths:
- Myth: “I’m young, so my bones are fine.” Truth: Bone loss starts silently in your 40s and 50s, especially with diabetes.
- Myth: “If my A1c is under 7%, I’m safe.” Truth: Even well-controlled diabetes increases fracture risk due to poor bone quality.
- Myth: “Walking is enough.” Truth: Walking doesn’t build bone strength. You need impact and resistance.
- Myth: “More calcium = stronger bones.” Truth: Too much calcium from pills can cause kidney stones or artery calcification. Food is safer.
Final Thought: Your Bones Are Part of Your Diabetes Management
Managing type 2 diabetes isn’t just about numbers on a glucose meter. It’s about protecting every part of your body-including your skeleton. Strong bones mean independence. They mean you can keep walking, climbing stairs, playing with grandkids, and living without fear of a fall. It’s not about perfection. It’s about consistency. Move. Eat well. Sleep. Avoid smoking. Check your levels. Talk to your doctor. Small steps, every day, add up to a lifetime of stronger bones.
Can type 2 diabetes cause osteoporosis?
Yes, type 2 diabetes increases the risk of osteoporosis, but not always in the way you expect. While bone density scans may show normal or high numbers, the actual quality of the bone is often poor. High blood sugar damages collagen, reduces bone formation, and increases inflammation-all of which make bones more fragile. This is called diabetic osteoporosis, and it leads to more fractures even when bone density looks okay.
Should people with type 2 diabetes take calcium supplements?
Not necessarily. Most people can get enough calcium from food-yogurt, leafy greens, canned fish with bones, and fortified plant milks. Supplements are only needed if you’re not getting enough from diet or if your doctor finds a deficiency. Too much calcium from pills can raise the risk of kidney stones or calcified arteries, especially in diabetics. Always check your vitamin D levels first, since your body needs it to absorb calcium properly.
Which diabetes medications are safest for bone health?
Metformin and GLP-1 agonists like semaglutide (Ozempic) and liraglutide (Victoza) appear to be neutral or even protective for bones. Thiazolidinediones (pioglitazone, rosiglitazone) should be avoided if you have low bone density or a history of fractures. SGLT2 inhibitors may slightly increase fracture risk in older adults, especially women. Always discuss your bone health with your doctor before starting or changing any diabetes medication.
Is walking enough to strengthen bones if I have type 2 diabetes?
Walking helps maintain bone density but doesn’t build it. To strengthen bones, you need weight-bearing and resistance exercises-like squats, lunges, lifting light weights, or using resistance bands. A 2023 study showed that people with type 2 diabetes who did strength training twice a week improved bone density by 3.5% in six months. Walking alone won’t give you that benefit.
How often should someone with type 2 diabetes get a bone density scan?
The American Diabetes Association recommends a bone density scan (DXA) for women over 65 and men over 70 with type 2 diabetes. But if you’re over 50 and have other risk factors-like a past fracture, low body weight, smoking, or long-term steroid use-you should ask for a scan earlier. Even if your A1c is well-controlled, bone quality can still be compromised. Don’t wait for a fall to get checked.
Can losing weight improve bone health in type 2 diabetes?
It depends on how you lose it. Losing fat through diet and exercise can reduce inflammation and improve bone quality. But losing too much weight too fast-especially muscle mass-can weaken bones. The goal is to lose fat while keeping or building muscle. Strength training during weight loss is key. People who lose weight without exercise often see a drop in bone density. Focus on body composition, not just the scale.


13 Comments
Kevin Jones
18 November, 2025Diabetic osteoporosis isn't a myth-it's a metabolic betrayal. High glucose cross-links collagen fibrils, creating brittle, non-plastic bone architecture. DXA scans measure mineral density, not microstructural integrity. You're not osteoporotic-you're osteodystrophic. The real villain? Insulin resistance starving osteoblasts of anabolic signals. No supplement fixes this. Only mechanotransduction via resistance loading reactivates Wnt/β-catenin signaling. Period.
Premanka Goswami
19 November, 2025They don't want you to know this-but Big Pharma replaced calcium with metformin because bones don't generate profit. The FDA approved thiazolidinediones knowing they turn marrow into fat. Your 'bone scan' is a lie. They scan density, not quality. And your doctor? He's on their payroll. Wake up. The real cure? Sunlight. Grounding. And quitting insulin-dependent treatments. Your bones are screaming. Are you listening?
Alexis Paredes Gallego
21 November, 2025Wait-so you're telling me the same meds that 'fix' your blood sugar are secretly turning your skeleton into chalk? And the doctors are just shrugging? That's not medicine. That's chemical sabotage. I've seen this before. Same playbook as the opioid crisis. They give you a drug that treats one symptom, then quietly destroy your whole system. You think you're healthy because your A1c is 'good'? Nah. You're just a walking fracture waiting to happen. And they'll sell you another pill to fix the fallout.
Saket Sharma
23 November, 2025Let’s be clear: walking is a placebo for lazy people. Bone remodeling requires mechanical overload-minimum 70% 1RM. Bodyweight squats? Child’s play. You need barbells. Heavy. Slow. Controlled. No cardio delusions. And vitamin D? If you’re not getting 5,000 IU daily from sun or supplement, you’re functionally deficient. Your bone turnover markers are garbage. Stop blaming genetics. Start lifting.
Shravan Jain
24 November, 2025the thing is... most of this is just common sense... but why do we need a 3000 word essay to tell us to lift weights and stop smoking? also... i think the study they cited? it was funded by a pharma company that sells resistance bands. just sayin'. and why no mention of magnesium? everyone forgets magnesium. bone health is 40% magnesium. not calcium. not vitamin d. magnesium. but nope. not in the article. typical.
Brandon Lowi
24 November, 2025America’s got the best healthcare money can buy-until you’re diabetic and your bones turn to dust. Then suddenly, you’re a statistic. They’ll give you a pill that makes you fat, then another pill to fix the side effects, then a third to fix the third pill’s side effects. Meanwhile, your femur’s crumbling. We need to stop outsourcing health to Big Pharma and start rebuilding our bodies with sweat, sunlight, and stubbornness. This isn’t medicine-it’s corporate triage.
Joshua Casella
26 November, 2025I’ve been working with diabetic patients for 15 years. The most common mistake? Thinking bone health is passive. It’s not. It’s active, daily, non-negotiable. I’ve seen 70-year-olds with A1c 8.5% who never broke a bone because they lifted weights three times a week. I’ve seen 55-year-olds with A1c 6.1% who shattered their hip from a step-off. It’s not about numbers. It’s about movement. If you’re reading this, stand up right now. Do three bodyweight squats. That’s your first step. Not tomorrow. Now.
Richard Couron
26 November, 2025They’re lying about the scans. I know. I work in radiology. The machine doesn’t see collagen degradation. It sees calcium. So if you’re eating calcium pills and sitting on your butt, your scan looks fine. But your bones? They’re like cardboard in a hurricane. And the drugs? SGLT2 inhibitors? They flush calcium out your pee. You think that’s safe? They’re selling you a death sentence with a 10% discount. Don’t trust the system. Trust your body. And if you’re falling? You’re already too late.
Alex Boozan
27 November, 2025Let’s cut through the noise. Bone health in T2D is a systems failure. You can’t fix it with isolated interventions. It’s glucose toxicity + insulin resistance + inflammation + sedentary lifestyle + vitamin D deficiency + medication side effects. You need a full-stack reset: resistance training, circadian lighting, protein timing, glycemic control, and zero processed sugar. No single pill. No magic food. Just relentless, boring consistency. If you’re looking for a shortcut, you’re already broken.
mithun mohanta
28 November, 2025Oh wow. Another ‘expert’ telling us to lift weights. How original. I mean, I’ve read about this in 17 peer-reviewed journals-none of which were written by people who actually have diabetes. Also, the author mentions ‘Maria from Sydney’-but never says if she’s on metformin or if her insulin levels were checked. This is amateur hour. Real science? It’s about osteocalcin carboxylation and RANKL/OPG ratios. Not ‘do squats.’ Please. I’ve got a PhD in biochemistry and even I’m embarrassed.
Evan Brady
29 November, 2025For real: if you’re over 50 and diabetic, get a FRAX score. It’s free. It tells you your 10-year fracture risk. Then get a DXA. Then find a physical therapist who knows diabetes. Don’t wait for a fall. Don’t wait for your doctor to bring it up. You’re the only one who cares about your body. Do the work. Start with heel raises. Do 10 every morning before coffee. Then add wall push-ups. Then a resistance band. Tiny steps. Daily. That’s how you rebuild. Not supplements. Not pills. Not magic. Just you, showing up.
Kevin Jones
1 December, 2025FRAX is a risk estimator, not a diagnostic. It’s calibrated for non-diabetic populations. In T2D, it underestimates fracture risk by up to 40%. You need quantitative ultrasound or HR-pQCT for true microarchitectural assessment. And collagen cross-links? They’re the real biomarker. CTx is outdated. Look for PINP and sclerostin. That’s where the real insight lies. The rest? Noise.
Evan Brady
3 December, 2025Right. And if you’re not a researcher with access to HR-pQCT machines, what do you do? You do the next best thing. You move. You eat protein. You get sunlight. You sleep. You don’t wait for perfect data to start living. Most people die waiting for the perfect plan. I’ve seen it. You don’t need a PhD to lift a dumbbell. You just need to start.