Blood Pressure Meds: What They Are, How They Work, and What to Watch For
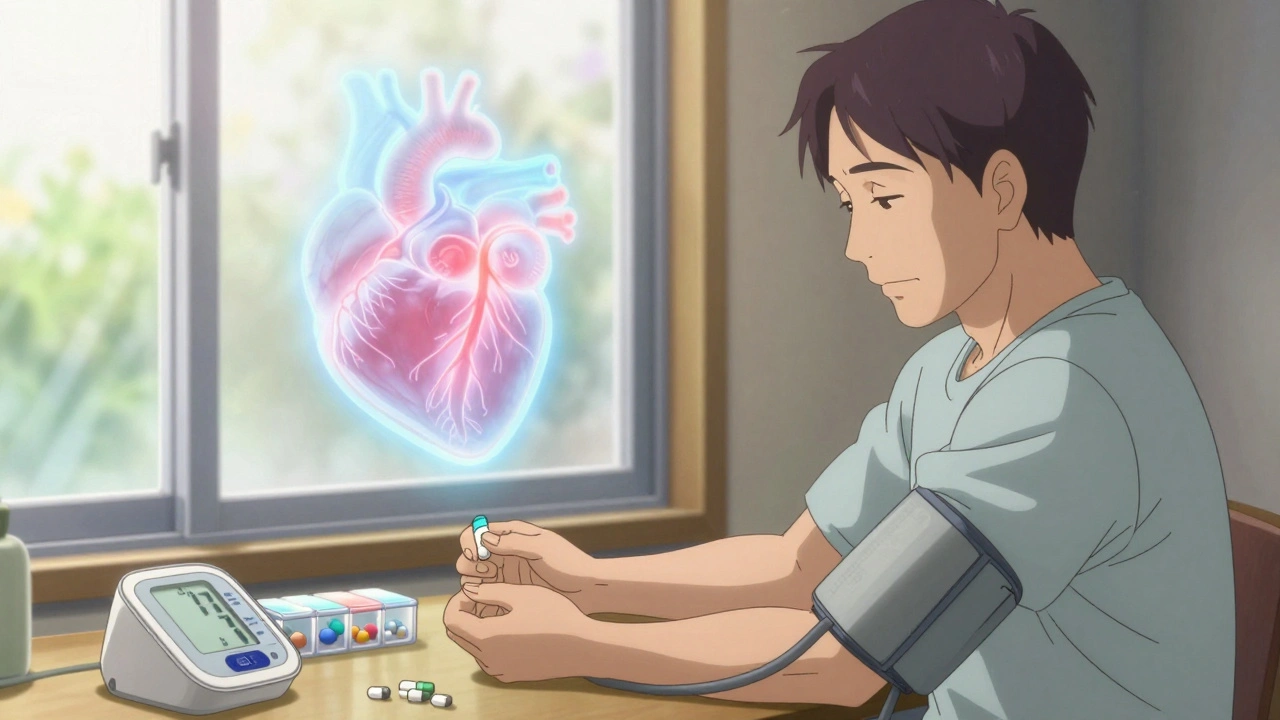
When your doctor says you need blood pressure meds, prescription drugs designed to lower elevated arterial pressure and reduce risk of heart attack or stroke. Also known as antihypertensives, these medications don’t cure high blood pressure—they help manage it every day, like insulin for diabetes. Skipping doses or mixing them with the wrong supplements can undo years of progress. It’s not just about popping a pill. What you take, when you take it, and what else you’re using all matter.
Many people on blood pressure meds, prescription drugs designed to lower elevated arterial pressure and reduce risk of heart attack or stroke. Also known as antihypertensives, these medications don’t cure high blood pressure—they help manage it every day, like insulin for diabetes. are also taking vitamin E, a fat-soluble antioxidant often used for skin health and immune support. Also known as alpha-tocopherol, it’s common in multivitamins and supplements. But high doses can increase bleeding risk, especially when paired with blood thinners. That’s why drug interactions, when two or more substances affect each other’s effects in the body, sometimes dangerously. Also known as medication conflicts, they can turn a safe routine into a health emergency. matter. The same goes for fish oil, a supplement rich in omega-3 fatty acids often taken for heart and brain health. Also known as omega-3 supplements, it’s popular but not risk-free when combined with certain blood pressure drugs.. You might think it’s all natural, so it’s safe—but it can thin your blood just like aspirin. Combine that with a beta-blocker or ACE inhibitor, and you’re playing with fire.
And it’s not just supplements. Even common cold meds can wreck your blood pressure control. Decongestants like pseudoephedrine can spike your numbers fast, especially if you’ve got an enlarged prostate or kidney issues. That’s why knowing what’s in every pill, capsule, or tea matters. Your pharmacist isn’t just filling prescriptions—they’re your last line of defense against dangerous combos.
Some people worry about side effects—dizziness, fatigue, cough, swollen ankles. Those are real, but they’re not universal. Often, switching to a different class of blood pressure meds fixes it. Maybe you need a diuretic instead of a calcium channel blocker. Or maybe your body just needs time to adjust. The key is talking to your doctor, not stopping cold turkey.
What you’ll find below isn’t a list of every drug on the market. It’s a collection of real, practical stories and warnings from people who’ve been there: the guy who nearly had a stroke because he took turmeric with his blood thinner, the woman who thought her memory issues were aging but were actually from statins, the man who didn’t know his herbal tea was raising his BP. These aren’t theoretical risks. They’re lived experiences. And they’re all connected to how you take your meds.