Calcium Channel Blockers: What They Are, How They Work, and What You Need to Know
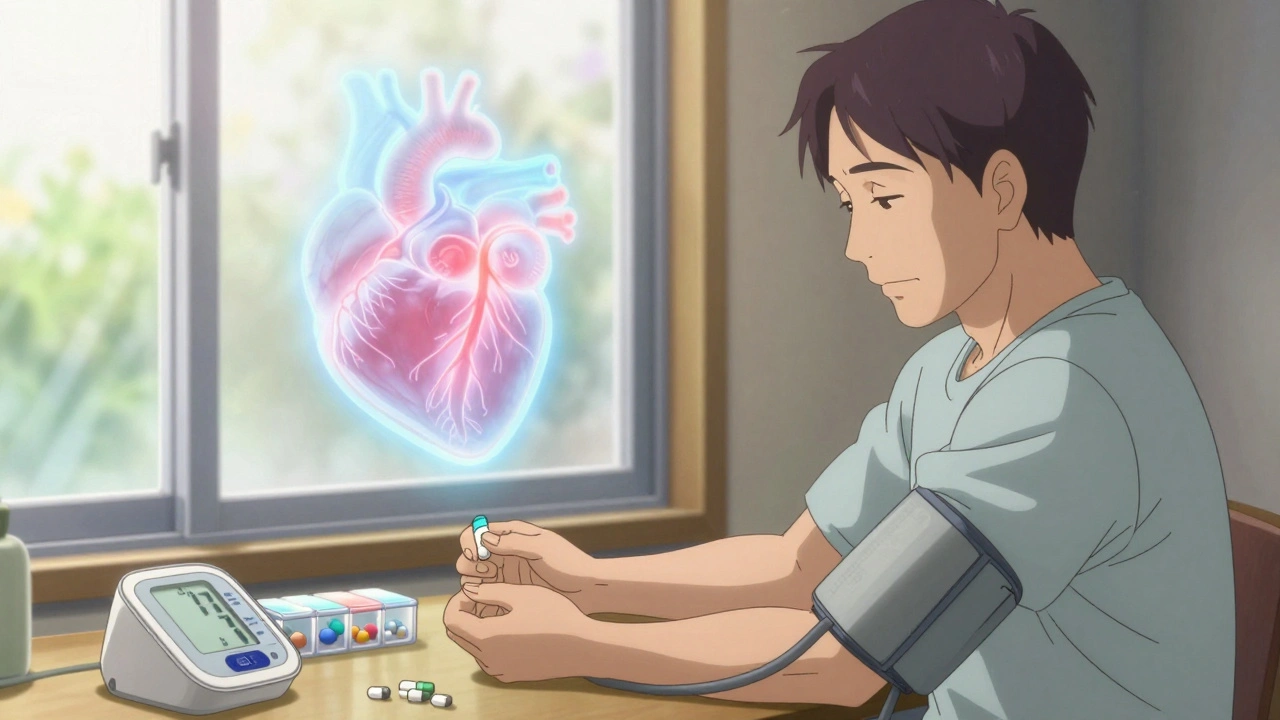
When your heart or blood vessels are working too hard, calcium channel blockers, a class of medications that prevent calcium from entering heart and blood vessel cells, reducing strain and lowering blood pressure. Also known as calcium antagonists, they’re one of the most common prescriptions for high blood pressure and chest pain. These drugs don’t just lower numbers—they help your body breathe easier, reduce heart strain, and prevent complications like strokes or heart attacks.
Calcium channel blockers work by blocking the flow of calcium into muscle cells in your heart and arteries. Less calcium means less contraction, so your arteries relax and widen, and your heart doesn’t have to pump as hard. That’s why they’re used for hypertension, a condition where blood pressure stays too high, putting stress on arteries and organs, angina, chest pain caused by reduced blood flow to the heart, and even some types of irregular heartbeat. They’re often prescribed when other meds like ACE inhibitors or beta blockers don’t work well—or when side effects are too much. Common types include amlodipine, diltiazem, and verapamil, each with slightly different effects on your heart or blood vessels.
But they don’t work in isolation. Many people on calcium channel blockers are also taking statins, cholesterol-lowering drugs that can interact dangerously with certain calcium blockers, especially if you’re on an antifungal or grapefruit juice. That’s why drug interactions, when one medication changes how another works in your body matter so much. A simple mix can raise your risk of muscle damage, low blood pressure, or kidney issues. That’s also why documenting your full list of meds—like in the article on medication documentation—isn’t just good practice, it’s life-saving.
These drugs aren’t for everyone. If you have heart failure with reduced pumping ability, certain types of calcium channel blockers can make it worse. And if you’re taking something like calcium acetate, a phosphate binder used in kidney disease, too much calcium from supplements or diet can push your levels into dangerous territory. That’s why monitoring your labs and talking to your doctor about what you’re taking is critical.
You’ll find real-world stories here—not just theory. People who’ve struggled with side effects, switched meds after muscle pain, or learned how to manage their treatment alongside other conditions like diabetes or kidney disease. You’ll see how polypharmacy, taking multiple medications at once affects your risk, how to spot early warning signs of interactions, and what to ask your pharmacist when a new script comes in. Whether you’re new to these meds or have been on them for years, the articles below give you the practical, no-fluff info you need to stay safe and in control.